When you take an antidepressant like Lexapro or Prozac, your brain is already working hard to keep serotonin levels steady. Now imagine adding a supplement like L-tryptophan on top of that. It sounds simple-more precursor, more serotonin, right? But here’s the catch: mixing L-tryptophan with certain antidepressants can push your serotonin system into dangerous territory. This isn’t theoretical. People have ended up in emergency rooms because of it.
What L-Tryptophan Actually Does in Your Brain
L-tryptophan isn’t just another amino acid you get from turkey or eggs. It’s the only building block your body uses to make serotonin-the brain chemical linked to mood, sleep, and calm. Without it, serotonin can’t be made. That’s why it’s been studied since the 1970s as a potential tool for depression.
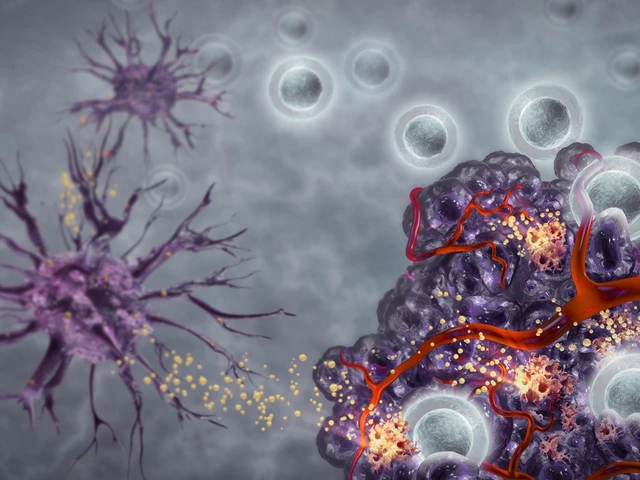
The process is straightforward but tightly controlled: L-tryptophan crosses the blood-brain barrier, gets converted to 5-HTP by an enzyme called tryptophan hydroxylase, then turned into serotonin by another enzyme. The amount of serotonin your brain produces depends almost entirely on how much tryptophan is available in your blood. Studies show that if you drop plasma tryptophan by 80%, serotonin production in the brain crashes by 95% within hours.
This isn’t just lab data. In real patients, when researchers use a technique called rapid tryptophan depletion (RTD)-giving a mix of amino acids that blocks tryptophan from entering the brain-nearly half of people on SSRIs relapse into depression within a day. Their mood drops, sleep gets worse, and anxiety spikes. It proves one thing: serotonin isn’t just a side player. It’s central to how these drugs work.
Why Some Antidepressants Are Riskier Than Others
Not all antidepressants play the same game with serotonin. SSRIs (like sertraline or fluoxetine) and MAOIs (like phenelzine) work by keeping serotonin around longer in the brain. Add L-tryptophan to that, and you’re basically pouring fuel on a fire. The result? Too much serotonin. That’s serotonin syndrome-a condition that can cause tremors, confusion, rapid heart rate, and in severe cases, seizures or death.
But here’s where it gets interesting: tricyclic antidepressants (TCAs) like amitriptyline behave differently. Early studies showed they actually boosted the brain’s response to tryptophan. That’s why some doctors used to combine them with tryptophan supplements in the 80s and 90s. But even then, it was risky. And today? Most psychiatrists avoid it.
Then there’s bupropion (Wellbutrin). It doesn’t touch serotonin at all. It works on dopamine and norepinephrine. So if you’re on bupropion, adding L-tryptophan won’t trigger serotonin syndrome. That’s a key distinction. If you’re considering supplementation, knowing which class of antidepressant you’re on isn’t optional-it’s life-saving.
The Dark History of L-Tryptophan Supplements
Back in 1989, the U.S. FDA banned L-tryptophan supplements. Not because the amino acid itself was dangerous-but because a single contaminated batch caused over 1,500 cases of eosinophilia-myalgia syndrome (EMS), a rare and deadly condition that attacks muscles, nerves, and skin. Thirty-seven people died. The culprit? A toxic byproduct from a poorly manufactured batch in Japan.
The ban stayed in place until 2005. During that time, research stalled. Scientists couldn’t study it. Doctors couldn’t prescribe it. And the public lost trust. When supplements returned, they came back with warnings-but not always clear ones. A 2021 FDA inspection found that 41% of tryptophan products on the market didn’t even mention serotonin syndrome as a risk.
Today, you can buy L-tryptophan online, in health stores, even on Amazon. But labels rarely say: “Do not use if you’re on an SSRI.” They say things like “Supports mood and sleep.” That’s not just misleading-it’s dangerous.
Who Should Never Take L-Tryptophan With Antidepressants
If you’re on an SSRI, SNRI, or MAOI, don’t take L-tryptophan. Period. That’s the rule from 73% of psychiatrists surveyed on Sermo in 2022. Why? Because the interaction is unpredictable. One person might feel fine. Another might spiral into serotonin syndrome within hours.
Even if you’re not on medication, you might still be at risk. People with a history of depression, anxiety, or bipolar disorder have what researchers call “serotonergic vulnerability.” In studies, these individuals saw their mood drop 3.2 times more than others after tryptophan depletion. That means their brains are already running on thin margins. Adding extra tryptophan could push them over the edge.
And it’s not just about mood. A 2009 study found that tryptophan depletion increased impulsive aggression by 28% in teens with ADHD. That’s a red flag for anyone with a history of emotional dysregulation.
What About Safe Dosing? Is There a Safe Amount?
The European Food Safety Authority says 5 grams per day is the upper safe limit for healthy adults. But that’s for people not on antidepressants. For someone on an SSRI? Even 500 mg a day has triggered symptoms in some users.
Real-world data from Reddit’s r/antidepressants community shows that 68% of users who took 500-1,000 mg of L-tryptophan reported better sleep. That sounds great-until you hear the other 22% describe nausea, dizziness, and racing thoughts. And 15% of Amazon reviews mention serotonin syndrome concerns. These aren’t outliers. They’re warning signs.
Some doctors do use tryptophan as an add-on for patients who aren’t responding fully to SSRIs. But they don’t wing it. They wait at least 7-10 days after stopping the SSRI. They monitor plasma tryptophan levels. They keep doses between 1-3 grams per day. And they only do it under strict supervision. This isn’t something you try at home.

What You Should Do Instead
If you’re on an antidepressant and feeling like it’s not working well enough, don’t reach for a supplement. Talk to your doctor. There are proven options: adjusting your dose, switching medications, adding therapy, or trying evidence-based alternatives like exercise, light therapy, or omega-3s-all with better safety profiles.
If you’re taking L-tryptophan for sleep or mood and you’re also on an antidepressant, stop immediately. Write down what you’ve been taking, how much, and when. Bring that list to your next appointment. Don’t assume your doctor knows you’re using it. Most patients don’t mention supplements unless asked.
And if you’re thinking about starting L-tryptophan because you read it helps with depression? Know this: the science is mixed. A major 2022 review of over 116,000 people found no solid proof that low serotonin causes depression. That means tryptophan might help some people-but not because it’s fixing a “chemical imbalance.” It might help because it improves sleep, reduces inflammation, or supports gut health. Those are real benefits. But they’re not the same as treating depression.
Bottom Line: Don’t Risk It
L-tryptophan isn’t harmless. It’s a powerful biochemical tool. And when you mix it with antidepressants, you’re playing with fire. The risks aren’t theoretical. They’re documented in peer-reviewed journals, FDA reports, and real patient stories.
If you’re not on an antidepressant, talk to your doctor before taking it. If you are? Don’t take it at all. There are safer, better-studied ways to support your mental health. Your brain doesn’t need extra serotonin-it needs stability. And the fastest way to lose that is by mixing supplements with prescription meds.
When it comes to your mental health, don’t guess. Don’t scroll. Don’t assume. Ask your doctor. Then listen.
Can I take L-tryptophan with SSRIs like Prozac or Zoloft?
No. Combining L-tryptophan with SSRIs significantly increases the risk of serotonin syndrome-a potentially life-threatening condition. Even low doses (500 mg) have triggered symptoms in sensitive individuals. This interaction is well-documented in clinical studies and strongly discouraged by psychiatrists.
What antidepressants are safest to use with L-tryptophan?
Bupropion (Wellbutrin) is the only common antidepressant that doesn’t affect serotonin levels. It works on dopamine and norepinephrine instead. So if you’re on bupropion, L-tryptophan doesn’t carry the same serotonin syndrome risk. But even then, consult your doctor before combining them.
How long should I wait after stopping an SSRI before taking L-tryptophan?
Most clinical guidelines recommend a 7-10 day washout period after stopping an SSRI before starting L-tryptophan. This allows the drug to fully clear from your system. For fluoxetine (Prozac), which stays in the body longer, wait at least 14 days. Never self-adjust timing-always follow your doctor’s guidance.
Is L-tryptophan better than 5-HTP for depression?
Neither is recommended as a standalone treatment for depression. Both are precursors to serotonin, but 5-HTP skips the first conversion step, making it more potent-and potentially riskier. Neither has strong evidence for treating depression on its own, and both carry the same interaction risks with antidepressants. Stick to proven therapies unless under medical supervision.
Why do some people say L-tryptophan helps their sleep?
L-tryptophan is also a precursor to melatonin, the hormone that regulates sleep. In people without serotonin-related conditions, low doses (500-1,000 mg) taken at night may improve sleep onset and quality. But if you’re on an antidepressant, the serotonin interaction can override this benefit and cause side effects like nausea, dizziness, or agitation.
What should I do if I think I have serotonin syndrome?
Seek emergency medical help immediately. Symptoms include high fever, rapid heart rate, muscle rigidity, confusion, seizures, or loss of consciousness. Stop all supplements and antidepressants until evaluated. Serotonin syndrome can escalate quickly-do not wait to see if it gets better.
For those considering L-tryptophan, remember: supplements aren’t regulated like drugs. Labels lie. Risks are hidden. And your brain doesn’t need more serotonin-it needs balance. If you’re struggling with mood or sleep, talk to a professional. There are safer paths forward.








Katelyn Sykes
17 Nov, 2025
L-tryptophan with SSRIs is a hard no and I’m tired of people treating it like a chill sleep hack
Gabe Solack
18 Nov, 2025
Just had a friend go to the ER over this 😣
She took 1g of tryptophan with her Zoloft for ‘better sleep’
Next thing she knows, she’s shaking, sweating, and hearing voices
Turns out she didn’t even know SSRIs affect serotonin
Doctors said she was 2 hours away from seizures
Now she’s on bupropion and doesn’t touch supplements
Don’t be her
🧠💀
Sarah Frey
19 Nov, 2025
Thank you for this comprehensive breakdown. As a mental health nurse, I see far too many patients self-medicating with supplements without understanding pharmacokinetics. The FDA’s 2021 inspection finding that 41% of products omit serotonin syndrome warnings is not just negligent-it’s a public health failure. Many patients assume ‘natural’ equals ‘safe,’ and this misconception leads to preventable hospitalizations. Education must be prioritized, not just in clinics but in supplement marketing. We owe it to our patients to demand transparency.
Kristina Williams
21 Nov, 2025
They banned tryptophan in '89 because Big Pharma didn't want people curing depression for $10 a bottle
Now they're selling SSRIs for $400 a month and calling it science
Ask yourself: who profits from you being scared of supplements?
The FDA? The AMA? Or the same people who told you smoking was safe?
They control the narrative. They control the data. They control your mind.
Don't be fooled.
Yash Nair
22 Nov, 2025
USA always overreacting
India uses tryptophan with antidepressants for decades
no one dies here
your doctors are scared of natural things
we eat eggs and milk daily
why you make problem for simple thing
your system is broken
Girish Pai
23 Nov, 2025
Let’s be clear: serotonin syndrome is a pharmacodynamic cascade resulting from excessive 5-HT1A and 5-HT2A receptor agonism secondary to monoaminergic potentiation. Tryptophan, as a rate-limiting precursor, synergizes with SSRIs to amplify synaptic serotonin concentration beyond the autoregulatory threshold. This is not anecdotal-it’s neuropharmacology 101. If you’re not familiar with the SERT transporter kinetics or the CYP450 metabolic profile of fluoxetine, you shouldn’t be self-prescribing amino acid supplements. Period.
Kristi Joy
23 Nov, 2025
I want to say thank you to everyone who’s shared their stories here
It takes courage to talk about mental health
But I also want to remind you-you’re not alone
If you’re scared to talk to your doctor, start with a text
‘Hey, I’ve been taking tryptophan for sleep and I’m worried’
That’s enough
You don’t need to be an expert
You just need to care enough to ask
And that’s already a win
Hal Nicholas
24 Nov, 2025
Of course you’re going to get serotonin syndrome
People take supplements like they’re gummy vitamins
They don’t read labels
They don’t research
They just see ‘natural mood booster’ and think it’s like taking vitamin D
Meanwhile, their brain is a ticking time bomb
And then they blame the system
It’s not the system
It’s the laziness
Stop being a sheep
Louie Amour
25 Nov, 2025
Let’s be honest-most people who take tryptophan are just looking for a quick fix because they don’t want to do the real work
Therapy? Too hard
Exercise? Too much effort
Changing sleep hygiene? Nah
But hey, popping a $12 capsule? That’s easy
And then they wonder why they’re still depressed
Supplements are the placebo of the modern age
And you’re all buying into it
Pathetic
Shilpi Tiwari
27 Nov, 2025
Interesting point about the tryptophan hydroxylase kinetics
But what about the gut-brain axis modulation via IDO pathway?
Recent studies suggest tryptophan diversion toward kynurenine under chronic inflammation may blunt serotonergic effects
So perhaps the risk profile isn’t linear
And if someone has high CRP and low tryptophan
Wouldn’t targeted supplementation actually restore balance?
Maybe we need personalized biomarkers, not blanket bans
Christine Eslinger
27 Nov, 2025
I’ve been on an SSRI for 7 years
I tried tryptophan once-just 500mg at night
Woke up at 3am with my heart pounding like I’d run a marathon
My hands were trembling
I thought I was having a heart attack
Turns out it was serotonin overload
My doctor said I got lucky
It could’ve been worse
Now I use magnesium glycinate and a consistent bedtime routine
My sleep is better
And I didn’t risk my brain
Sometimes the safest thing isn’t the most exciting thing
It’s the quiet choice
Denny Sucipto
29 Nov, 2025
Man I used to take tryptophan for sleep like it was nothing
Then I found out my cousin ended up in the hospital after mixing it with his Zoloft
He was fine after a few days
But he still gets panic attacks thinking about it
Now I tell everyone I know
If you’re on antidepressants
Don’t touch it
Not even a little
It’s not worth it
Trust me
Holly Powell
29 Nov, 2025
It’s fascinating how the public conflates biochemical precursors with therapeutic efficacy
There’s a fundamental epistemological flaw in assuming that increasing substrate concentration will linearly enhance neurotransmitter function
Neurotransmission is not a faucet
It’s a dynamic, homeostatically regulated system
And the notion that ‘more serotonin = better mood’ is a reductionist myth perpetuated by pharmaceutical marketing and wellness influencers
Until we deconstruct this serotonin myth, we’ll keep seeing preventable iatrogenic harm
Emanuel Jalba
30 Nov, 2025
THEY DON’T WANT YOU TO KNOW THIS
They banned tryptophan because it’s cheaper than Prozac
They’re scared you’ll figure out you don’t need their drugs
They’re scared you’ll heal yourself
They’re scared you’ll wake up
They’re scared you’ll stop paying $500 a month
They’re scared you’ll stop trusting them
Don’t be fooled
They’re lying to you
🙏🔥