When a drug goes straight into your bloodstream, there’s no room for error. Unlike pills that pass through your stomach and liver, injectables bypass every natural defense. One contaminated vial can cause sepsis, organ failure, or death. That’s why sterile manufacturing for injectables isn’t just about cleanliness-it’s about survival.
Why Sterility Isn’t Optional
In the 1920s, contaminated insulin killed patients. In 1955, a faulty polio vaccine caused paralysis in hundreds. The 2012 meningitis outbreak linked to contaminated steroid injections killed 64 people and sickened 751. These weren’t accidents. They were failures in sterile manufacturing. The standard today is clear: the chance of a single microorganism surviving in a vial of injectable must be less than one in a million. That’s called a Sterility Assurance Level (SAL) of 10-6. It’s not a suggestion. It’s a legal requirement under FDA 21 CFR Parts 210 and 211, EU GMP Annex 1 (2022), and WHO guidelines. No oral medication has this level of risk. A pill with a few bacteria? Your stomach acid kills it. An injection with one bacterium? That’s a medical emergency.Two Ways to Achieve Sterility
There are only two approved methods to make injectables sterile: terminal sterilization and aseptic processing. Terminal sterilization means you fill the vial, seal it, then kill everything inside with heat or radiation. Steam at 121°C for 15-20 minutes is the gold standard. It’s cheap, reliable, and gives you a SAL of 10-12-better than the required 10-6. But here’s the catch: only 30-40% of injectables can survive this. Biologics like monoclonal antibodies, vaccines, and protein-based drugs break down under heat. They’re too delicate. That’s where aseptic processing comes in. No heat. No radiation. Instead, everything-the drug, the vials, the stoppers, the air, the workers-is kept sterile from start to finish. This method is used for 60-70% of new injectables, especially biologics. But it’s far more complex.The Cleanroom Hierarchy
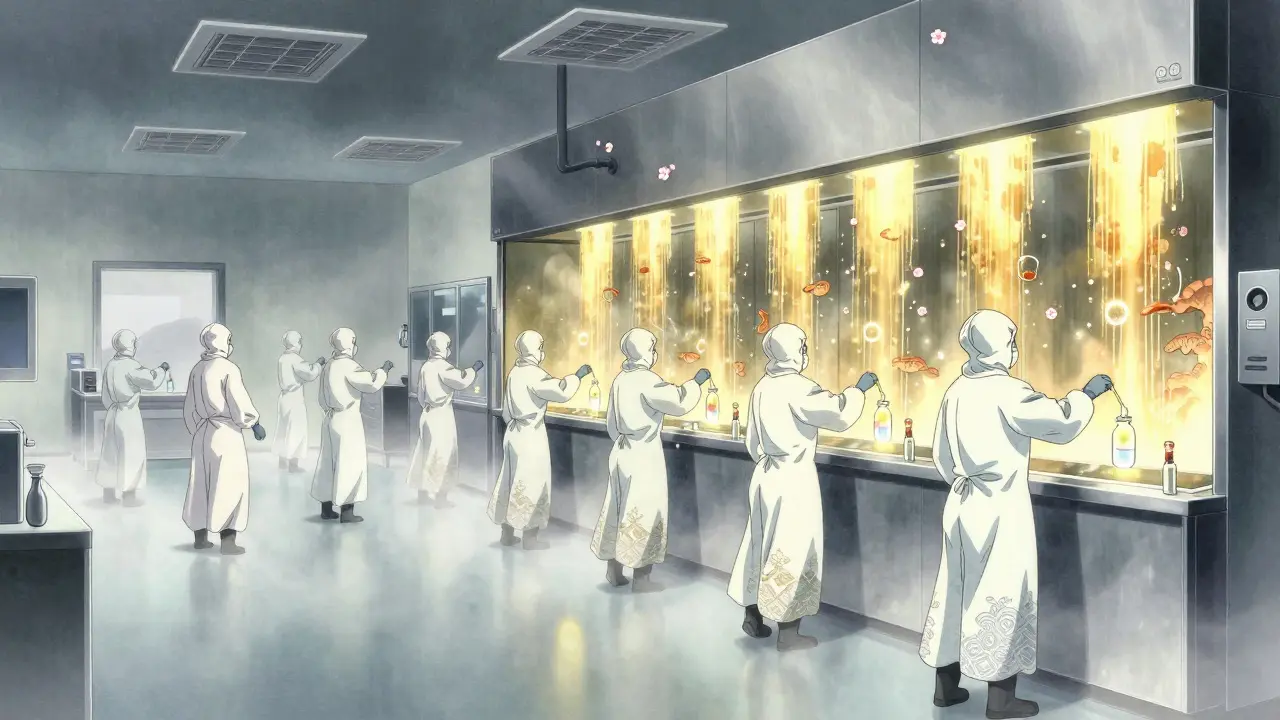
Aseptic processing doesn’t happen in a regular lab. It happens in cleanrooms built like spaceships. You start in an ISO 8 room (Class 100,000)-where workers gown up, wash hands, and put on sterile suits. Then you move to ISO 7 (Class 10,000) for mixing and preparing solutions. Finally, you enter the ISO 5 zone (Class 100)-the heart of the operation. This is where the drug is filled into vials. In this room, you’re allowed fewer than 3,520 particles per cubic meter that are 0.5 microns or larger. That’s less dust than you’d find in a typical home after vacuuming. Air moves in one direction, at 0.3-0.5 meters per second, like a silent waterfall. It’s not just filtered-it’s constantly replaced. Air changes happen 20 to 60 times per hour. Pressure is kept 10-15 Pascals higher than surrounding rooms so contaminated air can’t sneak in. Temperature? 20-24°C. Humidity? 45-55%. Too dry, and static electricity pulls particles into the product. Too wet, and mold grows.Water, Containers, and Pyrogens
The water used in injectables isn’t tap water. It’s Water for Injection (WFI)-purified to remove not just microbes, but endotoxins. The limit? Less than 0.25 Endotoxin Units per milliliter (EU/mL), as defined by USP <85>. Glass vials and rubber stoppers aren’t just cleaned. They’re depyrogenated. That means baked at 250°C for 30 minutes or more. Why? Because dead bacteria still release toxins-pyrogens-that cause fever and shock. Heat kills the bugs, but only extreme heat destroys the poison they leave behind. Container closure integrity is just as critical. A tiny leak, invisible to the eye, lets microbes in after production. Testing requires detecting leaks as small as 10-6 mbar·L/s using helium mass spectrometry. One vial with a leak can contaminate an entire batch.
Aseptic vs. Terminal: The Real Costs
Terminal sterilization costs about $50,000 per batch for a 1,000L run. Aseptic processing? $120,000 to $150,000. Why the gap? Aseptic facilities need isolators or RABS (Restricted Access Barrier Systems). Isolators are sealed, glove-box-like chambers where operators never directly touch the product. RABS are semi-enclosed workstations with laminar airflow. Both require expensive air handling, continuous monitoring, and highly trained staff. Isolators reduce contamination risk by 100 to 1,000 times compared to open cleanrooms, but cost 40% more to install. RABS are cheaper but demand stricter operator discipline. A 2023 study found isolators achieved 0.01 CFU/m³ in air samples. RABS hit 0.1 CFU/m³. Both meet standards-but isolators give you more margin for error.Media Fills: The Test That Saves Lives
Every six months, manufacturers run a media fill. They replace the drug with nutrient broth, run the entire filling process as if it were real, then incubate the vials for 14 days. If any vial grows bacteria, the whole process fails. The FDA requires 5,000 to 10,000 units per media fill. Why so many? Because if you only test 100 vials and one is contaminated, you can’t be sure it wasn’t a fluke. With 10,000 vials, a single failure is a red flag. A failure rate above 0.1% means your process isn’t under control. In 2022, 68% of FDA inspection deficiencies in sterile manufacturing were linked to media fill failures or aseptic technique errors. Not equipment. Not air filters. Human error. One manager on the PDA LinkedIn group reported three media fill failures in one quarter-costing $450,000 in lost batches. The cause? A tiny tear in a glove.People Are the Biggest Risk
No matter how perfect the machine, the human is the weak link. Workers must complete 40-80 hours of aseptic technique training. They’re requalified every six months. They move slowly. They don’t talk. They don’t make sudden movements. They wear full-body suits, masks, hoods, and double gloves. Even then, mistakes happen. A 2022 survey of 45 sterile facilities found 68% had at least one sterility test failure per year. Average cost per failure? $1.2 million. Training isn’t just about skill. It’s about mindset. A single lapse-reaching over a sterile field, turning your back to the product, skipping a disinfection step-can ruin everything.
Technology Is Changing the Game
New tools are reducing human error. Automated visual inspection systems now catch defects at 0.05%-down from 0.2%. That’s a 75% improvement. But it cost $2.5 million to install. Closed processing systems, where the drug flows from one sealed unit to another without human contact, are now used in 65% of new facilities. That’s up from 30% in 2018. Real-time monitoring is replacing periodic checks. Particle counters and microbial air samplers now run 24/7. If the air hits 1 CFU/m³, it’s an alert. At 5 CFU/m³, production stops. These systems caught 45% more deviations in a Lonza case study-and cut batch release time by 30%. Rapid microbiological methods are cutting test times from two weeks to 24 hours. That means faster releases and less inventory tied up.What’s Next?
The global sterile injectables market hit $225 billion in 2023 and is growing at 8.2% a year. Biologics-mostly monoclonal antibodies-are driving most of that growth. Over 40% of new drugs today require sterile injection. Regulations are tightening. EU Annex 1 (2022) demands continuous monitoring, risk-based approaches, and digital records. The FDA’s 2024-2026 plan includes AI tools to predict failures before they happen. But here’s the reality: building a sterile manufacturing line costs $50-100 million. Upgrading to meet Annex 1 adds $15-25 million. Most companies outsource to CDMOs like Catalent, Lonza, or Thermo Fisher. Today, 55% of sterile injectables are made by contract manufacturers. For smaller players, the bar is high. In 2022, only 28 of 1,200 Chinese sterile facilities passed FDA inspections. Regulatory compliance isn’t optional-it’s the price of entry.Final Takeaway
Sterile manufacturing for injectables isn’t about being clean. It’s about being flawless. Every step-from water purity to worker movement to air pressure-must be controlled, documented, and validated. One mistake can kill. The systems in place aren’t perfect, but they’re the best we have. The future belongs to those who invest not just in equipment, but in culture: training, discipline, and constant vigilance. Because when a drug enters your blood, there’s no second chance.What is the difference between terminal sterilization and aseptic processing?
Terminal sterilization kills microbes after the product is sealed, using heat or radiation. It’s reliable and cheaper, but only works for products that can handle high temperatures-about 30-40% of injectables. Aseptic processing keeps everything sterile during manufacturing without using heat. It’s used for heat-sensitive drugs like biologics, but requires advanced cleanrooms, strict procedures, and constant monitoring. Aseptic is more expensive and complex, but necessary for most modern injectables.
Why are cleanrooms classified by ISO levels?
ISO classifications define how clean a room is based on particle count per cubic meter. ISO 8 is the least clean (used for gowning), ISO 5 is the cleanest (used for filling). Each level has strict limits on airborne particles. This system ensures contamination risk drops as you get closer to the product. ISO 5 rooms must have fewer than 3,520 particles ≥0.5μm per cubic meter. Higher levels mean lower risk of contamination.
What is a media fill, and why is it required?
A media fill is a simulated production run where sterile broth replaces the actual drug. The entire filling process is done exactly as if producing real product. Afterward, vials are incubated for 14 days to see if any microbes grow. If they do, the process fails. Media fills prove the system works under real conditions. The FDA requires 5,000-10,000 units per simulation to catch rare failures. It’s the most important test for aseptic processes.
How do you prevent pyrogens in injectables?
Pyrogens-fever-causing toxins from dead bacteria-are removed by depyrogenation. Glass vials and stoppers are baked at 250°C for at least 30 minutes. This destroys endotoxins that survive regular sterilization. Water for Injection (WFI) must also meet strict limits: less than 0.25 EU/mL. Raw materials are tested for bioburden, and only materials with fewer than 10 CFU/g are allowed in non-sterile steps.
What are the biggest causes of sterile manufacturing failures?
The top causes are human error, environmental monitoring gaps, and media fill failures. FDA data shows 68% of deficiencies relate to aseptic technique-like improper gowning, glove tears, or reaching over sterile zones. Thirty-seven percent of inspections found inadequate environmental monitoring. Twenty-eight percent cited media fill failures. Training, continuous monitoring, and automation are the best defenses.








Monte Pareek
18 Dec, 2025
Let me tell you something about sterile manufacturing that nobody talks about - it’s not the machines or the cleanrooms that fail, it’s the humans who think they’re invincible. I’ve seen techs in ISO 5 zones scratch their noses through their masks, then act like nothing happened. And the media fills? They’re not just tests - they’re the last line of defense. One glove tear, one lapse in focus, and suddenly you’re responsible for six dead people. The cost isn’t just financial - it’s moral. Every dollar spent on training, every second spent monitoring air flow, every minute spent requalifying staff - that’s the price of not killing someone. This isn’t manufacturing. It’s sacred duty.
Nicole Rutherford
19 Dec, 2025
So let me get this straight - you’re telling me we’re spending $100 million to make sure a vial doesn’t have a single bacteria… but we still let people walk in wearing socks and flip-flops outside the facility? Yeah right. This whole system is a placebo. They’re just scared of lawsuits. If you really wanted to prevent contamination, you’d automate everything and ban humans from the room. But no - we need the ‘human touch’ so we can feel better about ourselves while we risk lives. Wake up.
Dorine Anthony
21 Dec, 2025
Wow. This is actually one of the most sobering things I’ve read all week. I used to think ‘sterile’ just meant clean. Now I realize it means ‘no room for even the tiniest mistake.’ I’m gonna think twice before complaining about my IV getting a little cold next time.
Elaine Douglass
22 Dec, 2025
Thank you for writing this. I had a relative who got sepsis from a contaminated injection years ago. They never found out how it happened. Reading this made me understand why they never got answers - because the system is so fragile, and so quiet, until it breaks. Please keep sharing stuff like this. People need to know.
Anna Sedervay
23 Dec, 2025
It is my professional opinion, as a certified pharmaceutical compliance officer with dual accreditation from the FDA and EMA, that the current regulatory framework is not merely inadequate - it is fundamentally archaic. The reliance upon ISO classifications, which were developed in the 1980s, fails to account for the micro-aerosol dynamics of modern biologics. Furthermore, the 10^-6 SAL is a statistical fiction; biological systems do not operate on probabilistic models, they operate on deterministic failure modes. Until we adopt quantum-level particulate detection and real-time genomic contamination mapping, we are merely performing theatrical compliance. And let us not forget: the 2022 EU Annex 1 mandates digital twin validation - yet 87% of facilities still use paper logs. This is not manufacturing. This is medieval ritual.
James Stearns
24 Dec, 2025
It is imperative that we acknowledge the inherent contradiction in the industry’s approach. We demand perfection, yet we permit human operators to enter the sterile zone after consuming coffee, which contains microbial biofilm residues. The fact that gloves are still the primary barrier is an affront to scientific integrity. I propose, as a matter of urgent ethical obligation, the immediate implementation of full-body exoskeletal robotic manipulation systems - operated remotely by certified technicians in geographically isolated bunkers. Anything less is negligence dressed as innovation.
William Storrs
26 Dec, 2025
Anna, I hear you - and you’re right. The system is fragile. But here’s the thing - we don’t need to fix everything at once. We just need to fix one thing at a time. That glove tear? Train the team on glove inspection protocols. That media fill failure? Run a weekly shadowing session with senior operators. Progress isn’t about perfection. It’s about consistency. Every time someone catches a mistake before it becomes a disaster, that’s a life saved. Keep pushing. We’re all in this together.
Mark Able
26 Dec, 2025
Wait - so if one vial has a leak, the whole batch is ruined? Then why do we even make more than one vial at a time? Just make one. One vial. One patient. One chance. Done. Why are we still doing batch production? This is 2025. We have 3D printers. We can print a sterile syringe with the drug inside it, right now, for one person. Why are we still using glass vials from the 1950s? Someone explain this to me.