Desensitization Protocol Selector
Select Your Scenario
Recommended Protocol
Critical Consideration
Additional Information
When a medication saves your life but also triggers a terrifying allergic reaction, what do you do? For many patients, the answer isn’t avoiding the drug-it’s desensitization. This isn’t a workaround or a band-aid. It’s a medically supervised process that lets your body temporarily tolerate a drug you’re allergic to, so you can get the treatment you need. And it works-often with near-perfect success.
What Desensitization Actually Does
Desensitization isn’t about curing your allergy. It’s about creating a temporary window where your immune system stops overreacting to a specific drug. Think of it like slowly turning up the volume on a speaker until your ears adjust. You’re not changing the drug. You’re changing how your body responds to it-just for that one course of treatment. The process works best for immediate, IgE-mediated reactions: hives, swelling, trouble breathing, low blood pressure, or anaphylaxis that happens within minutes to an hour after taking the drug. These are the kinds of reactions that make doctors say, “We can’t give you this again.” But if that drug is the only one that works-like penicillin for a stubborn bone infection or paclitaxel for advanced cancer-desensitization becomes the only real option. Studies from Brigham and Women’s Hospital show success rates of 95% to 100% when done right. In one group of 42 patients with penicillin allergies, every single one completed their full antibiotic course after desensitization. No deaths. No anaphylaxis. Just mild flushing or itching in a few cases. That’s not luck. That’s science.When It’s the Only Choice
You don’t desensitize just because you’re allergic. You do it when there’s no alternative. Take antibiotics. Penicillin is one of the most effective, cheapest, and safest drugs for infections like osteomyelitis or endocarditis. But up to 10% of people report a penicillin allergy-even though most of them aren’t truly allergic. Still, if you’ve had a real reaction, doctors avoid it. That’s where substitution comes in: switching to a different antibiotic. But here’s the problem: 15-20% of those substitutes don’t work as well. Some are more toxic. Others are less effective against the exact bacteria you have. And cross-reactivity? It’s real. If you’re allergic to penicillin, you might also react to cephalosporins. That leaves you with fewer options than you think. Now consider chemotherapy. Drugs like carboplatin, paclitaxel, and rituximab are lifesavers for cancer patients. But up to 20% of people develop hypersensitivity reactions to them after a few doses. Stopping treatment means risking cancer progression. Switching drugs might mean lower survival rates. Desensitization lets patients keep their best treatment. In one study, 92% of oncology patients called it “life-saving.” Premedication with antihistamines and steroids sounds safer-but it fails. In one trial, 10% of chemotherapy patients still had severe reactions despite premedication. Desensitization cut that risk to under 2% when done properly.The Two Main Types of Protocols
There are two main ways to do this: rapid and slow. Rapid Drug Desensitization (RDD) is used for immediate reactions. It’s done intravenously, usually over 4 to 6 hours. The process starts with a tiny dose-1/10,000th of the full dose-and doubles every 15 minutes. By the end, you’ve received the full therapeutic dose. This protocol was standardized at Brigham and Women’s Hospital and is now used worldwide. It’s the go-to for antibiotics, monoclonal antibodies, and many chemotherapies. Slow Drug Desensitization (SDD) is for delayed reactions-those that show up days later with rashes, fever, or organ inflammation. These are T-cell mediated, not IgE. The process takes longer: hours or even days. Oral aspirin desensitization, for example, might start with 10 mg and increase every 60 to 90 minutes over two or three days. There’s no universal rule for SDD yet. Dosing varies by drug, reaction type, and patient history. Route matters too. IV is most common for antibiotics (70% of cases). Oral is standard for aspirin and NSAIDs. The timing between doses is stricter for oral: 60+ minutes, versus 15-30 minutes for IV.What Happens During the Procedure
This isn’t something you do at home. Not even close. Every step is monitored. Blood pressure, oxygen levels, heart rate, and breathing are checked before, during, and after each dose. Nurses and allergists stay with you the whole time. The room has emergency equipment ready: epinephrine, IV fluids, oxygen, ventilators. If you react-say, you break out in hives or your blood pressure drops-the dose is paused. Medications are given to calm the reaction. Once you’re stable, they might continue, but more slowly. In rare cases, they stop entirely. But in properly run centers, severe reactions happen in less than 2% of cases. The key? Training. Only allergists and immunologists with specific experience should run these protocols. A 2020 study found that 8% of errors came from incorrect drug dilutions. That’s not a small mistake. That’s life-threatening.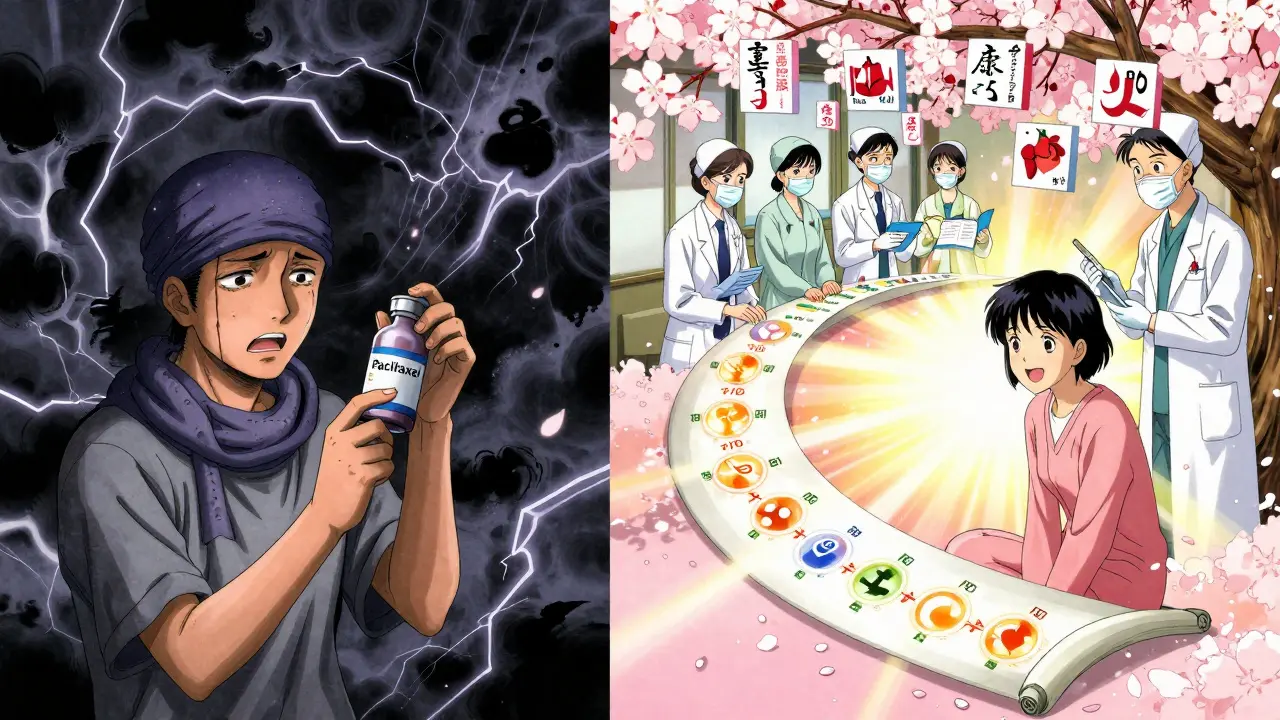
Who Shouldn’t Try It
Desensitization isn’t for everyone. It’s strongly discouraged for people who’ve had severe delayed reactions like Stevens-Johnson syndrome or toxic epidermal necrolysis. These are rare but deadly skin conditions. The risk of triggering them again is too high. The American Academy of Allergy, Asthma & Immunology gives a clear “strong recommendation against” desensitization in these cases. It also doesn’t work well for 30-40% of delayed hypersensitivity reactions. If your reaction came days after taking the drug, and it wasn’t an immediate anaphylactic event, desensitization might not help. Alternatives should be explored first. And if you’re not in a hospital or specialized center? Don’t even consider it. Community clinics without proper equipment, staff, or protocols have three times the complication rate. One Reddit user described a hospital that didn’t have the right dilution kits-“took 3 attempts before they got it right.” That’s not a minor hiccup. That’s a danger zone.Why It’s Becoming More Common
The world is changing. Antibiotic resistance is killing 35,000 people a year in the U.S. alone. Many of those infections could be treated with older, cheaper antibiotics-like penicillin-if patients weren’t labeled allergic. Desensitization unlocks those options. Cancer drugs are getting more complex. New biologics and monoclonal antibodies often come with high allergy risks. Without desensitization, many patients would lose access to the most effective treatments. The market is growing. The global desensitization market hit $1.2 billion in 2022 and is expected to grow nearly 13% a year through 2030. Academic hospitals have adoption rates over 85%. Community hospitals? Only 35%. The gap isn’t just about money-it’s about training, equipment, and confidence.The Hidden Costs and Challenges
This isn’t a cheap or simple procedure. Each session takes 4.2 nursing hours and 1.8 physician hours. That’s a full workday for a team. Medicare only covers about 60% of the actual cost. Many small hospitals can’t afford it. Training is another barrier. Allergists need to supervise 15 to 20 procedures before they’re considered proficient. Mistakes in patient selection happen in 15% of community cases. Protocol deviations? 22% in non-specialized centers. Solutions are emerging. Standardized dilution kits cut preparation errors by 75%. Electronic checklists reduce selection errors by 60%. Simulation training boosts protocol adherence from 78% to 96%. These aren’t luxuries-they’re necessities.
What Patients Say
The feedback from patients who’ve been through it is powerful. One person wrote on Reddit: “After 20 years of being labeled allergic, the 4-hour protocol let me finally take the best antibiotic for my osteomyelitis.” Another, a cancer survivor, said: “I didn’t think I’d survive another round of chemo. Desensitization gave me back my chance.” But anxiety is real. Sixty-three percent of patients report feeling terrified before the procedure. The long hours, the constant monitoring, the fear of a reaction-it’s intense. That’s why support, clear communication, and preparation matter just as much as the protocol itself.The Future: Personalized Desensitization
The next frontier isn’t just doing desensitization better-it’s knowing who needs it before you start. New research is using biomarkers like basophil activation tests to predict success with 89% accuracy. Genetic and immunologic profiling might soon tell us: “You’re a perfect candidate for rapid desensitization,” or “You’re better off avoiding this drug entirely.” Home-based protocols are in early trials-with 92% success so far. Imagine being able to complete your desensitization in your living room, under remote supervision. It’s not science fiction anymore. Dr. Mariana Castells, who helped pioneer these protocols, says: “Within five years, genetic and immunologic profiling will determine who needs desensitization and which protocol will succeed.” That’s not a prediction. It’s a roadmap.Final Takeaway
Desensitization isn’t a last resort. It’s a lifeline-for people with life-threatening infections, for cancer patients with no other options, for anyone who’s been told they can’t take a drug that could save them. It’s safe. It’s effective. But it’s not simple. It requires expertise, resources, and careful planning. If you or someone you know has a serious drug allergy and needs a critical medication, ask: “Is desensitization an option?” Don’t assume it’s too risky. The risk of not doing it might be higher.Can you desensitize to any drug?
No. Desensitization works best for IgE-mediated immediate reactions to drugs like penicillin, chemotherapy agents, monoclonal antibodies, and some antibiotics. It’s not effective for severe delayed reactions like Stevens-Johnson syndrome or toxic epidermal necrolysis. It also doesn’t work well for all drug classes-some lack proven protocols. Always consult an allergist or immunologist to determine if your specific drug and reaction type are suitable.
Is desensitization permanent?
No. The tolerance is temporary. Once you stop taking the drug for more than 24 to 72 hours (depending on the medication), your immune system can return to its allergic state. That means if you need the drug again in the future-even weeks later-you’ll need to go through the full desensitization process again. It’s not a cure, but a reset for each course of treatment.
Can my family doctor perform desensitization?
No. Desensitization must be performed by an allergist or immunologist in a hospital or specialized clinic equipped to handle anaphylaxis. It requires specific training, emergency equipment, and staff experienced in managing severe reactions. Attempting it in a general practice or outpatient setting without these resources significantly increases the risk of serious complications.
How long does a desensitization take?
It depends on the drug and protocol. Rapid desensitization for IV antibiotics or chemotherapy typically takes 4 to 6 hours. Slow desensitization for oral drugs like aspirin or NSAIDs can take 2 to 3 days, with doses spaced hours apart. The time is determined by the drug’s half-life, reaction type, and safety protocols.
What are the side effects during desensitization?
Mild reactions like flushing, itching, or a slight drop in blood pressure are common and expected. These are managed with antihistamines or other medications during the procedure. Severe reactions like anaphylaxis are rare-occurring in less than 2% of properly supervised cases. Most patients tolerate the process well, especially when the protocol is followed exactly and monitoring is continuous.
Is desensitization covered by insurance?
Medicare and most private insurers cover desensitization when medically necessary, but reimbursement often doesn’t cover the full cost-typically only about 60%. This financial gap makes it harder for smaller hospitals to offer the service. Patients should check with their provider and ask for prior authorization. Documentation showing no alternative therapies exist is often required.








Darren Links
22 Jan, 2026
So let me get this straight-America spends billions on this fancy desensitization crap while other countries just use cheaper antibiotics and live? We turn everything into a high-stakes medical drama. I get it, we love our overpriced healthcare theater, but this is just corporate medicine in a lab coat.
Kat Peterson
22 Jan, 2026
OMG I CRIED reading this 😭💔 I had chemo and they did this to me and I thought I was gonna DIE but then-like a miracle-I got my full dose and now I’m 5 years cancer-free 🌈✨ This isn’t just science, it’s *magic* with IV drips and nurses holding your hand 💖
Don Foster
24 Jan, 2026
The 95% success rate is misleading because they only include patients who didn’t have preexisting organ damage or comorbidities which means the real world success is probably more like 60-70% and even that’s generous because most studies are funded by pharma companies who profit from extended hospital stays
siva lingam
25 Jan, 2026
So you pay 10k to not die from penicillin but you could’ve just taken cipro for 50 bucks? Sounds like a scam designed by someone who owns a hospital.
Shelby Marcel
25 Jan, 2026
wait so if you get desensitized and then need the drug again in 3 weeks you have to do the whole thing over?? that sounds insane like why not just test if you’re still allergic first??
blackbelt security
25 Jan, 2026
This is why we need to stop treating medicine like a luxury. If a drug saves lives, it shouldn’t be locked behind a 6-hour hospital marathon. We need community protocols. We need training. We need to stop letting fear dictate care.
Tommy Sandri
26 Jan, 2026
The global disparity in access to desensitization protocols is a profound ethical concern. While academic centers in the United States report adoption rates exceeding 85%, many low-resource settings lack even the most basic infrastructure to support such interventions. This represents a systemic inequity in life-saving care.
Luke Davidson
28 Jan, 2026
I had this done for paclitaxel after my third round nearly killed me. They told me I was done. I cried in the parking lot. Then I begged them to try it. Four hours. Sweat. Shaking. But I got my full dose. And now I’m here. My kids still call me "Chemo Superdad." I’m not a hero. I just didn’t want to leave. This isn’t magic. It’s just people refusing to give up on you. And that? That’s everything.
Shanta Blank
28 Jan, 2026
Let’s be real-this whole thing is a money machine. You get a patient terrified of death, then you charge them for 4 hours of monitoring, $2000 in meds, and a team of specialists just so they can get a drug that’s been around since 1928. Meanwhile, insurance only pays 60%. Who’s really getting rich here? Not the patient. Not the nurse. The hospital admin who got a bonus for "increasing procedural volume."
John McGuirk
30 Jan, 2026
They say it’s safe but what if this is all a cover for Big Pharma to keep pushing expensive drugs? What if the real allergy is to generic meds? What if they’re making people think they need this so they keep buying branded chemo? I’ve seen the charts. The same companies fund the studies. The same people run the clinics. Coincidence? I don’t believe in coincidences.