Medication Safety Risk Estimator
This tool estimates your risk of medication errors based on factors documented in the article. Data shows marginalized communities face higher risks due to systemic barriers.
Enter Your Information
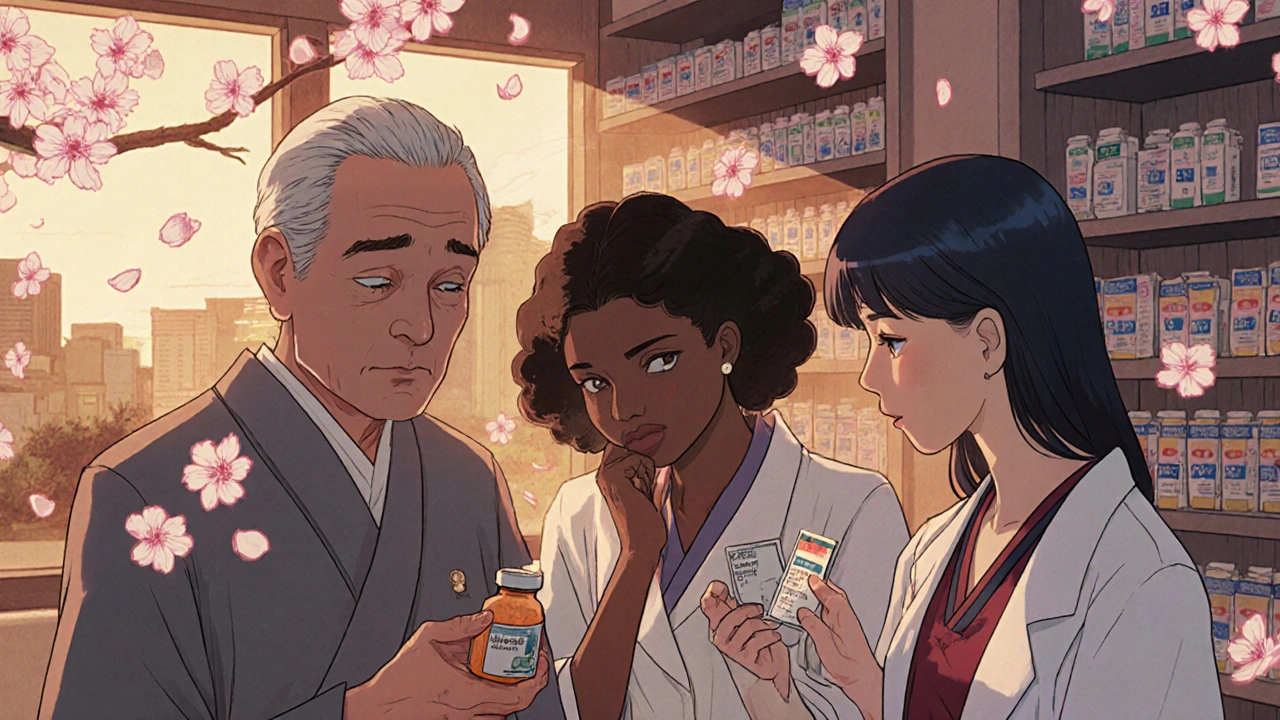
Every year, millions of people around the world suffer harm from medications that should have kept them safe. For some, it’s a simple mistake-a wrong dose, a missed warning. For others, it’s a system failure. And the worst part? These failures don’t hit everyone equally. People of color, older adults, non-English speakers, and low-income communities are far more likely to experience dangerous medication errors-and far less likely to have their concerns heard or documented. This isn’t bad luck. It’s systemic.
Medication Errors Don’t Happen in a Vacuum
The World Health Organization calls medication harm one of the top global patient safety issues. Their Medication Without Harm campaign, launched in 2017, aims to cut severe, avoidable medication-related harm by 50% within five years. The cost of these errors? Over $42 billion annually. But behind that number are real people-people who can’t afford their prescriptions, who don’t trust their doctors, or who don’t speak the language used in hospitals. A 2025 study across five NHS hospitals found that patients from white or Black ethnic backgrounds were more likely to have medication incidents reported than those from other minority groups. That doesn’t mean those groups have fewer errors. It means their errors go unnoticed. Why? Language barriers. Cultural mistrust. Clinicians assuming a patient doesn’t understand their own symptoms. A Black patient in Georgia told researchers that doctors often dismissed their pain as “emotional,” not physical. That’s not an isolated case. It’s a pattern.Who Gets Left Out of Clinical Trials?
New drugs are tested in clinical trials. But those trials rarely reflect the real world. From 2014 to 2021, Black Americans made up only about one-third of participants in trials for conditions they were most affected by. The same gap existed for Hispanic and Indigenous populations. Even during the COVID-19 vaccine trials-where diversity was a major talking point-Black people were still underrepresented compared to their share of the population. This isn’t just about fairness. It’s about safety. If a drug hasn’t been tested on your body type, your metabolism, or your genetic background, how do we know it won’t hurt you? In 2021, the U.S. Preventive Services Task Force couldn’t issue specific colorectal cancer screening guidelines for Black patients because there simply weren’t enough studies that included them. That’s not science. That’s neglect.Cost Blocks Access-And Safety
Even when a medication is proven safe and effective, many people can’t get it. In 2022, nearly 19% of Hispanic Americans and 11.5% of Black Americans were uninsured. That’s compared to 7.4% of White Americans. When you can’t afford your blood pressure pill, you skip doses. When you can’t pay for a new anticoagulant, you stick with an older, riskier one. That’s not choice. That’s survival. And when you can’t afford your meds, you turn to over-the-counter alternatives. A 2024 JAMA Network Open study found that people in underserved communities often rely on herbal supplements, expired prescriptions, or shared medications because they have no other option. These aren’t informed decisions-they’re desperate ones. And they lead to dangerous interactions, overdoses, and avoidable hospitalizations.
Biases in the Clinic Are Deadly
Implicit bias isn’t just a buzzword. It changes prescriptions. It changes dosages. It changes whether a patient’s complaint is taken seriously. A well-documented example: Black patients are consistently undertreated for pain. Studies show doctors are less likely to believe Black patients are in real pain, even when their symptoms match those of White patients. That leads to underprescribing of opioids, but also to underprescribing of safer alternatives because the pain isn’t seen as legitimate. The Agency for Healthcare Research and Quality (AHRQ) calls this a patient safety crisis-not a social one. Why? Because these disparities aren’t accidental. They’re built into how care is delivered. A doctor assumes a patient won’t understand complex instructions. A pharmacist skips explaining side effects because they think the patient won’t follow them. A nurse doesn’t double-check a dosage because they assume the family won’t notice. These aren’t malicious acts. They’re unconscious habits. And they’re deadly.Technology Can Help-Or Hurt
Electronic health records were supposed to fix this. But they often make disparities worse. Algorithms used to flag high-risk patients sometimes rely on historical data that includes biased practices. If Black patients were historically underprescribed certain drugs because of bias, the algorithm might assume they’re “low risk” now-even if their condition is worsening. That’s why the U.S. Office of the National Coordinator for Health Information Technology launched a $15 million initiative in 2024 to build AI tools that detect medication safety disparities in real time. These tools don’t just look at diagnoses. They look at race, income, language, insurance status, and prescription refill patterns. They ask: Is this patient getting the same level of safety checks as others? But tech alone won’t fix this. If we don’t fix the human side-the assumptions, the silence, the lack of cultural training-then we’re just automating bias.
What’s Being Done? And What’s Missing?
The Joint Commission now lists equity as a formal patient safety goal. That’s progress. The WHO includes equity as one of its four core domains in the Medication Without Harm framework. Good. But action is lagging. A 2024 survey by the American Hospital Association found that only 32% of U.S. hospitals have formal programs to address medication safety disparities-even though 78% say it’s a priority. That gap between recognition and action is huge. Some hospitals are trying. One in Chicago now hires bilingual medication safety advocates who walk patients through their prescriptions in their native language. Another in Texas uses community health workers to follow up with patients after discharge, checking if they understand their meds and can afford them. These aren’t fancy tech solutions. They’re human ones. But they’re rare. And they’re underfunded.How to Fix This-For Real
There’s no single fix. But there are clear steps that work:- Train clinicians in cultural humility, not just cultural competence. It’s not about memorizing traditions-it’s about listening without judgment.
- Expand professional interpretation services in every clinic and hospital. Not just phone interpreters-on-site, trained medical interpreters who know drug names and side effects.
- Collect and report demographic data with every medication error. If you don’t track who’s being harmed, you can’t fix it.
- Include diverse populations in clinical trials from day one-not as an afterthought, but as a requirement for approval.
- Reduce out-of-pocket costs for high-risk medications. No one should choose between food and their heart medication.
- Partner with community organizations. People trust their churches, their barbershops, their local nonprofits. Let them help design safety messages.
It’s Not Just a Health Issue. It’s a Justice Issue.
Medication safety isn’t just about pills and prescriptions. It’s about who gets to live safely. Who gets to be heard. Who gets to trust the system. When a Latina woman in Arizona can’t get her insulin because the pharmacy won’t accept her Medicaid card, that’s a medication safety failure. When an elderly Asian man in California doesn’t report his dizziness because he’s afraid of being called “confused,” that’s a medication safety failure. When a Black teenager in Detroit skips his asthma inhaler because he doesn’t want to be labeled “noncompliant,” that’s a medication safety failure. These aren’t edge cases. They’re the norm. And they’re preventable. The data is clear. The solutions exist. What’s missing is the will to change.Why are medication errors higher in marginalized communities?
Medication errors are higher in marginalized communities due to a mix of systemic barriers: lack of access to care, language differences, cultural mistrust, implicit bias from providers, and unaffordable medications. These factors lead to under-reporting, miscommunication, and unsafe medication use that isn’t caught by standard safety systems.
Do clinical trials include enough diverse participants?
No. From 2014 to 2021, Black Americans made up only about one-third of participants in clinical trials for conditions they were most affected by. Hispanic and Indigenous groups were similarly underrepresented. This means many drugs aren’t tested on the populations that need them most, leading to unsafe or ineffective use in real-world settings.
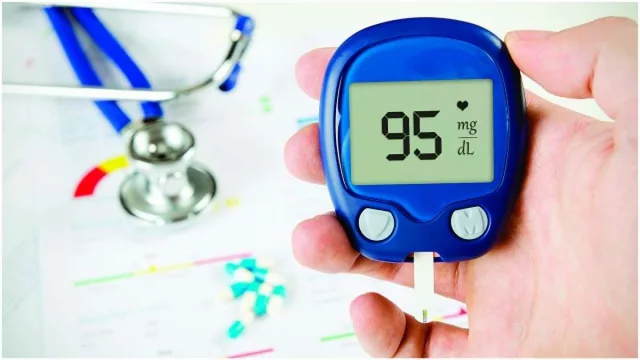
How does insurance status affect medication safety?
People without insurance are far more likely to skip doses, split pills, or use expired or shared medications because they can’t afford prescriptions. In 2022, 18.7% of Hispanic Americans and 11.5% of Black Americans were uninsured-compared to 7.4% of White Americans. This directly increases the risk of dangerous drug interactions and treatment failures.
Can AI help reduce medication safety disparities?
Yes, but only if designed carefully. AI tools can flag patterns like missed refills or inconsistent dosing across racial or income groups. But if they’re trained on biased historical data, they can reinforce those biases. The U.S. government launched a $15 million initiative in 2024 to build equitable AI tools that detect disparities in real time-not just predict risk.
What can hospitals do right now to improve medication safety equity?
Hospitals can start by hiring on-site medical interpreters, collecting demographic data with every medication error report, training staff in cultural humility, partnering with community organizations to deliver safety messages, and requiring diverse participation in clinical trials before approving new drugs. Simple, low-cost steps like these have already reduced errors in pilot programs across the U.S.









Olivia Currie
30 Nov, 2025
This hit me right in the chest. I worked in a clinic where a woman cried because she had to choose between her insulin and her daughter’s school supplies. This isn’t just policy-it’s people. We need to stop treating healthcare like a luxury and start treating it like a human right. #MedicationJustice
Curtis Ryan
1 Dec, 2025
bro i just saw a guy on tiktok say his grandpa died because he skipped his meds to pay rent… like… we’re literally letting people die because they’re poor?? this is insane. we need to fix this now. 😭
Rajiv Vyas
2 Dec, 2025
you think this is about race? nah. it’s about the globalist pharma cartel controlling everything. they don’t want you healthy-they want you dependent. clinical trials? fake. AI tools? surveillance. they’re using ‘disparities’ to push their agenda. the real solution? stop trusting hospitals. grow your own herbs. trust your gut.
farhiya jama
4 Dec, 2025
meh. i read this and just felt… tired. like, why do we keep talking about this? nothing ever changes. just give me my coffee and let me scroll.
Astro Service
5 Dec, 2025
we dont need no fancy interpreters or cultural training. we need americans to learn english and stop complaining. if you cant afford medicine go get a job. this is america. we dont coddle people. stop playing the victim card.
DENIS GOLD
6 Dec, 2025
oh wow, another ‘systemic racism’ sob story. next you’ll say the moon landing was faked because black people weren’t on the rocket. get over it. if you’re dumb enough to skip your meds because you’re ‘too poor,’ that’s on you. not the system. 🤡
Ifeoma Ezeokoli
7 Dec, 2025
i’ve seen this in my own family. my aunt in Lagos couldn’t get her hypertension meds because the pharmacy only stocked them in dollars. she traded yams for a few pills. we need to remember-this isn’t just about data. it’s about dignity. let’s lift each other up. 🤝
Daniel Rod
8 Dec, 2025
we’re all just trying to survive, right? 🌱 maybe the real question isn’t ‘how do we fix the system’… but ‘how do we stop treating people like problems to be managed’? i think healing starts when we stop looking at patients as cases and start seeing them as humans. with names. with stories. with fear. with hope. 💛
gina rodriguez
9 Dec, 2025
thank you for writing this. i work in a community pharmacy and see this every day. small things help-like writing dosing instructions in big letters, or just asking ‘can you afford this?’ like it’s normal. it’s not glamorous, but it saves lives. 🙏
Sue Barnes
11 Dec, 2025
if you can’t afford your meds, you shouldn’t be taking them. period. people who don’t follow instructions are a liability. this isn’t ‘unfair’-it’s common sense. stop blaming doctors for patients who refuse to be responsible.
jobin joshua
11 Dec, 2025
bro i got this one time i went to the hospital and the nurse said ‘you’re too dark for this pill’ 😂😂😂
Sachin Agnihotri
11 Dec, 2025
Wait-so you’re saying AI is biased because it uses historical data? But that’s how all algorithms work… unless we start from scratch with perfect data-which we can’t. So what’s the alternative? We need to fix the data, not the tool. And we need to do it fast.
Diana Askew
12 Dec, 2025
they’re using ‘equity’ to sneak in socialism. next they’ll mandate that every doctor must be bilingual. what about the ones who work 80-hour weeks? they’re not magic. this is just more government control. 🤦♀️
King Property
12 Dec, 2025
You think this is bad? Try living in a country where the government controls your meds. In China, they ration insulin based on your social credit score. In Russia, they use AI to predict who’s ‘noncompliant’ and cut their benefits. This isn’t a US problem-it’s a global collapse of the medical-industrial complex. You think your hospital is safe? They’re tracking your refill patterns. They know if you skipped your pills. They’re building your profile. And they’re not done yet. You’re already being watched.