When dealing with Alzheimer's dementia, a progressive neurodegenerative disorder that impairs memory, thinking, and behavior. Also known as senile dementia, it affects millions worldwide and drives a complex care ecosystem.
Understanding neurodegenerative disease, a class of conditions where nerve cells gradually lose function and die is key because Alzheimer's sits alongside Parkinson’s and Huntington’s as major examples. Neurodegenerative disease influences cognitive decline, the steady loss of mental abilities such as recall, reasoning, and language, which clinicians track with tools like MMSE and MoCA. Managing this decline often requires medication management, strategies to prescribe, monitor, and adjust drugs like donepezil, memantine, and newer disease‑modifying agents. Proper oversight reduces side effects and maximizes quality of life.
People with caregiver support, resources, training, and community networks that help families handle daily challenges form the backbone of long‑term care. Caregivers benefit from education on safety modifications, routine planning, and stress‑relief techniques. Studies show that early involvement in support groups can lower burnout rates by up to 30%. In addition, linking medication management with caregiver oversight creates a feedback loop: caregivers notice subtle changes, prompting timely dose adjustments.
These four pillars—Alzheimer's dementia itself, its neurodegenerative nature, the associated cognitive decline, and the combined effort of medication and caregiver support—are woven throughout the resources below. Below you’ll find practical guides, medication cost‑saving tips, and up‑to‑date research summaries that address each aspect. Dive in to see how each article ties back to these core concepts and helps you navigate the complex landscape of Alzheimer’s care.
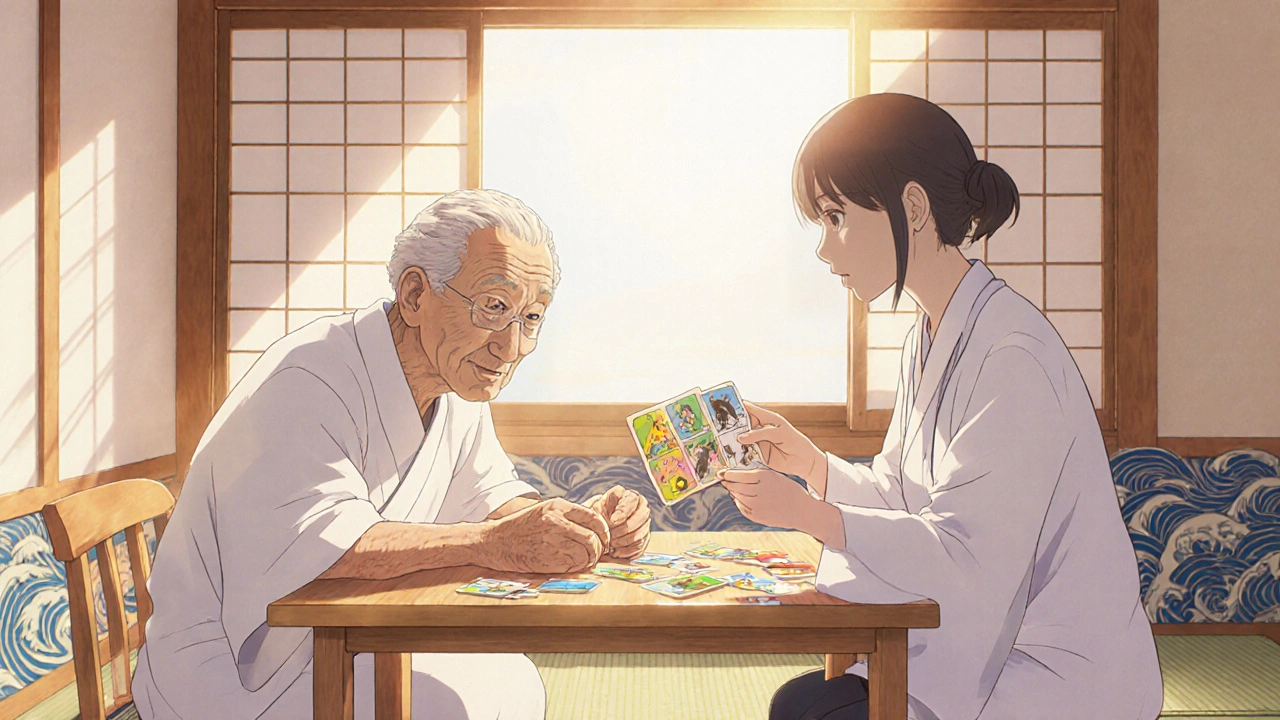
Learn how cognitive stimulation can slow Alzheimer's dementia, the science behind neuroplasticity, activity ideas, and practical steps to create an effective home program.
CONTINUE READING