A cerebral aneurysm isn’t something you hear about until it’s too late. Most people live with one for years without knowing. It’s a weak spot in a brain artery that bulges like a balloon, and if it bursts, it can cause a life-threatening bleed called a subarachnoid hemorrhage. About cerebral aneurysm cases are found accidentally during scans for other reasons. But knowing your risk - and what to do next - can make all the difference.
Who’s at Risk for a Rupture?
Not all brain aneurysms rupture. In fact, most don’t. But some have a much higher chance. Age is a big factor. If you’re over 65, your risk of rupture is nearly three times higher than someone in their 40s. Women are also more likely to develop them - about 1.6 times more often than men. And if two or more close family members have had one, your risk jumps fourfold. Genetics matter. Lifestyle choices play a huge role too. Smoking is the biggest modifiable risk. People who smoke now have over three times the risk of rupture compared to non-smokers. The more you smoke, the worse it gets - smoking 10 or more cigarettes a day raises your risk by nearly half. High blood pressure is just as dangerous. If your systolic pressure stays above 140 mmHg, your rupture risk nearly doubles. Heavy drinking - more than 14 drinks a week - adds another 32% risk.What Makes an Aneurysm More Likely to Burst?
Size matters, but not in the way you might think. An aneurysm larger than 7 mm has more than three times the risk of rupture compared to smaller ones. But even small ones can burst - especially if they’re in the wrong spot. Aneurysms at the anterior communicating artery (AComm) are notorious for rupturing even when they’re under 5 mm. These are among the most dangerous locations. Shape is just as important as size. Aneurysms with irregular bulges, lobes, or daughter sacs are far more unstable. These irregular shapes create turbulent blood flow that weakens the wall further. Studies show they carry almost three times the rupture risk compared to smooth, round ones. Location also changes the game. Aneurysms in the middle cerebral artery have a rupture risk nearly four times higher than those elsewhere. Blood flow patterns inside the aneurysm matter too. When blood moves slowly or swirls in chaotic directions, it puts stress on the vessel wall. Computational studies show that 83% of ruptured aneurysms had these abnormal flow patterns, compared to just 42% of unruptured ones. Inflammation inside the wall also plays a role. Higher levels of IL-6 and CRP - markers of inflammation - are found in people who’ve had ruptures.The PHASES Score: Your Personal Rupture Risk
Doctors don’t guess. They use tools. The PHASES score is the gold standard for predicting rupture risk over five years. It combines six factors: your population (region), blood pressure, age, aneurysm size, whether you’ve had a previous bleed, and where the aneurysm is located. Each factor adds points. A score of 0-3 means your 5-year rupture risk is only 3%. A score of 9-10? That’s 45%. Every single point increase raises your risk by 32%. That’s why even small changes - like quitting smoking or lowering your blood pressure - can shift your score enough to change your treatment plan. If your PHASES score is 6 or higher, most experts recommend treatment. Below that, monitoring may be safer.Treatment Options: Clipping, Coiling, or Flow Diversion
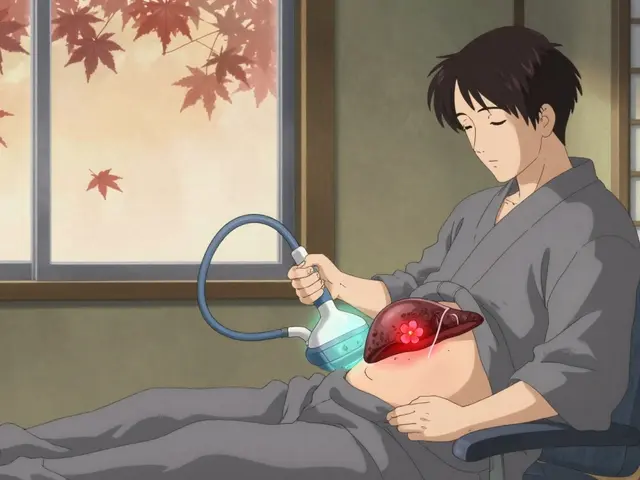
If your aneurysm is high-risk, you’ll need treatment. There are three main options. Surgical clipping is the oldest method. A neurosurgeon opens the skull, finds the aneurysm, and places a tiny titanium clip across its neck to stop blood flow into it. It’s a permanent fix - 95% of clipped aneurysms are completely sealed. But it’s invasive. Recovery takes weeks. People over 70 have a 35% higher chance of complications. Endovascular coiling is less invasive. A catheter is threaded from the groin up to the brain. Platinum coils are pushed into the aneurysm, causing it to clot off. Success rates are 78-85% at six months. It’s faster, less painful, and has lower mortality - 1.1% versus 1.5% for clipping. But it’s not always permanent. About 16% of coiled aneurysms need a second procedure within 12 years. Flow diversion is the newest option. It uses a special mesh stent - like the Pipeline Embolization Device - placed across the artery. Blood flows through the mesh, away from the aneurysm, letting it slowly shrink and seal over time. It’s ideal for large, wide-necked, or complex aneurysms. One-year occlusion rates hit 85.5% with newer models. But it requires long-term blood thinners and carries a slightly higher risk of delayed complications.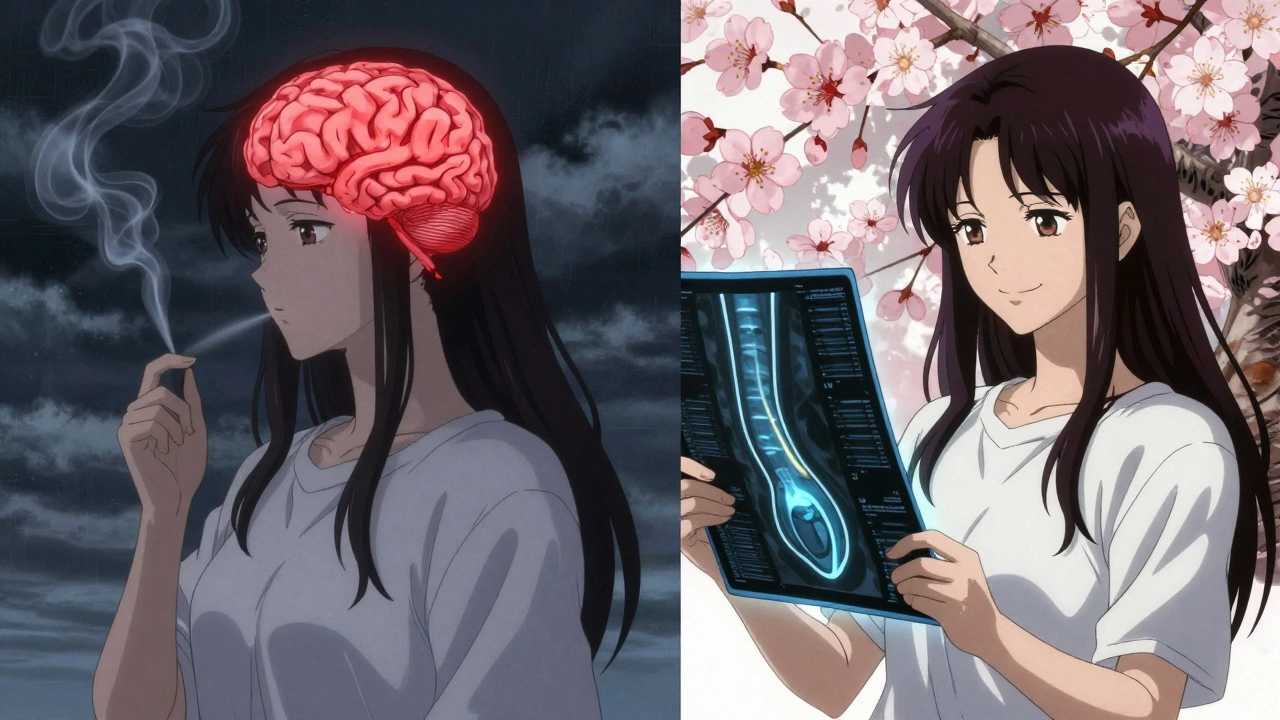
Which Treatment Is Right for You?
There’s no one-size-fits-all answer. It depends on your aneurysm’s shape, size, and location. A wide-necked aneurysm in the middle of a branch? Flow diversion is likely best. A small, rounded one near the front? Coiling might work fine. A large, irregular one in the back of the brain? Clipping may still be preferred because endovascular tools struggle there. Your age and health matter too. If you’re young and otherwise healthy, clipping offers a permanent solution. If you’re older or have other conditions like heart disease, coiling is usually safer. For patients with multiple aneurysms, the risk of rupture jumps nearly fourfold. That often pushes doctors toward treating the most dangerous one first.What If You Don’t Treat It?
Many small, low-risk aneurysms are just watched. The UCAS Japan study showed that aneurysms under 5 mm in the front of the brain have only a 0.2% chance of rupturing over five years. In the back, it’s 0.7%. That’s lower than the risk of a car accident on your daily commute. For these, the goal is prevention: control your blood pressure, quit smoking, cut back on alcohol, and get annual MRA scans to check for growth. If the aneurysm grows even 1 mm, your risk spikes. That’s when treatment usually becomes necessary.Long-Term Outcomes and Quality of Life
Successful treatment cuts your 10-year re-rupture risk from 68% down to just 2.3%. That’s the difference between living in fear and living normally. Quality of life after treatment also varies. People who get coiling report better scores on quality-of-life measures (EQ-5D: 0.82) compared to those who have surgery (0.76) at one year. They return to work faster, have less pain, and recover more fully. But long-term, all three treatments offer similar survival rates - if the aneurysm is successfully treated.
What’s Next in Research?
Scientists are working on better ways to predict rupture before it happens. The HUNT study found 17 genetic markers linked to aneurysm formation and rupture. Blood tests for these could one day identify high-risk people before an aneurysm even forms. Machine learning is also helping. New models analyze 42 different features - size, shape, flow patterns, wall thickness - to predict rupture risk more accurately than PHASES alone. These tools are still in testing, but they’re getting closer to clinical use.What Should You Do If You’re Diagnosed?
First, don’t panic. Most unruptured aneurysms don’t need immediate treatment. Second, work with a neurovascular specialist. Ask for your PHASES score. Ask about your aneurysm’s size, shape, and location. Ask whether growth has been seen on prior scans. Third, take control of what you can. Quit smoking - your rupture risk drops 54% within two years. Get your blood pressure under 130/80. Limit alcohol. Avoid heavy lifting or extreme stress that spikes blood pressure. And finally, get regular imaging. Annual MRA scans catch growth early. That’s when intervention is most effective and safest.Medical Management Is Part of the Treatment
Even if you’re not having surgery or coiling, medical care is essential. Blood pressure control isn’t optional - it’s life-saving. Smoking cessation isn’t just advice - it’s the single most effective way to lower your rupture risk. Alcohol moderation isn’t a suggestion - it’s a medical necessity. Medications like beta-blockers or ACE inhibitors may be prescribed to keep pressure stable. But no pill can replace quitting smoking or controlling your diet. These are the real treatments.When to Seek Help Immediately
If you suddenly get the worst headache of your life - described as "thunderclap" - call emergency services. Other signs: nausea, vomiting, stiff neck, blurred vision, or loss of consciousness. These could mean your aneurysm has ruptured. Survival drops 30-40% within the first 24 hours if treatment is delayed. Minutes matter.Can a cerebral aneurysm go away on its own?
No, a cerebral aneurysm won’t disappear without treatment. Once formed, it remains a weak spot in the artery. In rare cases, a small aneurysm may clot off naturally, but this is unpredictable and dangerous. Most require monitoring or intervention to prevent rupture. Never assume it will heal on its own.
Are all brain aneurysms dangerous?
No. Most cerebral aneurysms never rupture. About 3.2% of people have them, but only 9-10 per 100,000 rupture each year. Small, smooth, and low-risk aneurysms - especially under 5 mm and in the front of the brain - have very low rupture rates. The danger comes from size, shape, location, and risk factors like smoking or high blood pressure.
How often should I get scanned if I have an unruptured aneurysm?
Annual MRA (magnetic resonance angiography) scans are standard for unruptured aneurysms. If your aneurysm is small and stable, your doctor may space scans to every 1-2 years. But if it’s growing, changing shape, or you have a high PHASES score, scans may be needed every 6 months. Never skip follow-ups - growth is the biggest red flag.
Can I exercise with a cerebral aneurysm?
Yes - but carefully. Light to moderate exercise like walking, swimming, or cycling is safe and even encouraged. Avoid heavy lifting, intense weight training, or activities that cause sudden spikes in blood pressure. Always check with your doctor before starting a new routine. The goal is to keep your blood pressure steady, not to push it to the limit.
What’s the difference between coiling and clipping?
Clipping is open brain surgery. A surgeon places a metal clip across the aneurysm neck to block blood flow. It’s permanent but requires a long recovery. Coiling is minimally invasive. A catheter delivers platinum coils into the aneurysm to cause clotting. Recovery is faster, but retreatment is more common. Clipping has a 95% success rate; coiling is 78-85%. Your aneurysm’s shape and location determine which is better.
Does having one aneurysm mean I’ll get more?
About 20-30% of people with one cerebral aneurysm have more than one. If you have multiple, your rupture risk increases nearly fourfold. That’s why doctors scan the entire brain, not just the affected area. Genetic factors and long-term high blood pressure are the main reasons multiple aneurysms develop.
Can I fly with an unruptured cerebral aneurysm?
Yes, flying is generally safe for people with unruptured aneurysms. Cabin pressure changes during flights don’t significantly increase rupture risk. However, if you’ve recently had treatment or have a very large aneurysm, consult your neurologist first. Avoid long flights if you’re not cleared, and stay hydrated.
What’s the survival rate after a ruptured aneurysm?
About 30-40% of people die within the first 24 hours after a rupture. Of those who survive the initial bleed, about half will have long-term disabilities. Early treatment - within hours - improves survival. That’s why recognizing symptoms like a sudden, severe headache is critical. Every minute counts.











Akash Sharma
3 Dec, 2025
Man, I never realized how much genetics and lifestyle play into this. I had no idea smoking tripled your rupture risk - I quit two years ago after my uncle had a bleed, and honestly, I didn’t think it made that big a difference. But now I see it’s not just about avoiding the big stuff - it’s about stacking small wins. Lower BP, cut alcohol, skip the heavy lifting. It’s like building a dam one brick at a time. Also, the PHASES score thing? That’s actually genius. Doctors should show patients this like a credit score - simple, visual, actionable. Makes it feel less abstract.
Mark Gallagher
4 Dec, 2025
Incorrect. The article states that aneurysms under 5mm in the anterior circulation have a 0.2% five-year rupture risk. That is statistically insignificant. Yet, the author implies monitoring is sufficient - which is medically irresponsible. The data shows that even small aneurysms in high-flow zones like AComm can rupture. This is not a "wait and see" condition. You do not gamble with brain hemorrhages. The author is dangerously downplaying risk.
Wendy Chiridza
6 Dec, 2025
I appreciate the breakdown on coiling vs clipping but I wish they’d mentioned recovery timelines more clearly. I had coiling last year and honestly the first month was rough - not because of pain but because of the fatigue. People think "minimally invasive" means "back to normal in a week" but it’s not true. Also the follow-up MRA scans? They’re expensive and anxiety-inducing. Insurance shouldn’t make you jump through hoops for them.
Jessica Ainscough
7 Dec, 2025
Thank you for writing this. I’ve been living with a 4mm unruptured aneurysm for three years now. I used to panic every time I got a headache. Now I know most of them are just stress or dehydration. I quit smoking, started walking daily, and got my BP down to 125/78. I don’t feel like a ticking time bomb anymore. It’s not about fixing the aneurysm - it’s about fixing your life around it. And that’s something anyone can do.
Stacy Natanielle
8 Dec, 2025
So... you're telling me I need to stop drinking wine every night? 😔🍷 And quit my 2-pack-a-day habit? 😭 I just turned 67. Isn't it a little late? Also, why are they always talking about "risk"? Can't we just say "you might die"? That's what this is. Why sugarcoat it? 🤷♀️
kelly mckeown
8 Dec, 2025
i just found out i have a 3mm aneurysm last month and honestly i've been crying every night. i'm 41, i have two kids, and i keep thinking about what if i die before they're grown. i don't even know what to ask my doctor. i just want someone to tell me it's going to be okay. i'm scared
Tom Costello
10 Dec, 2025
As someone who grew up in a family where everyone smoked and drank, I never thought brain aneurysms were "my thing." But reading this, I realize how much culture plays into this. In my community, drinking is social, smoking is stress relief, and seeing a doctor is for "when you’re really sick." This isn’t just medical advice - it’s cultural change. We need outreach programs, not just pamphlets. Maybe partner with barbershops, churches, community centers. This info needs to reach people who don’t Google their symptoms.
dylan dowsett
12 Dec, 2025
Wait - so you’re saying if I have a 6mm aneurysm, and I’m 68, and I smoke, and my BP is 150/90, and it’s in the AComm - then I have a 45% chance of bleeding in 5 years? But you’re telling me to "monitor" it? That’s not monitoring - that’s waiting for a bomb to go off. And you call that medicine? I’ve seen too many people die from "watchful waiting." This is negligence dressed up as caution.
Susan Haboustak
12 Dec, 2025
The author says "most aneurysms don’t rupture" - true. But that’s like saying "most plane crashes don’t happen" - it doesn’t make flying safe if you’re the one on the plane. This article is dangerously optimistic. It ignores the psychological toll of living with a silent timer in your skull. The real risk isn’t just rupture - it’s the constant dread. No one talks about that. And no, "annual MRA scans" aren’t a cure. They’re a prison sentence.
Chad Kennedy
13 Dec, 2025
So... I gotta quit smoking? And stop drinking? And not lift my grandkids? What’s the point of living if I can’t do anything? I’m 59. I’ve had this thing for 10 years and I’m still here. Maybe I should just chill and enjoy my life. I’m not dying because of a little bulge. I’ve got better things to do than worry about my brain.
Siddharth Notani
13 Dec, 2025
Excellent summary. For those in India, access to MRA is limited. Many rely on CTA or ultrasound - which are less sensitive. If you cannot get regular imaging, prioritize BP control and smoking cessation above all. The PHASES score is valid globally. Do not delay quitting smoking - even in low-resource settings, this is the single most effective intervention. Stay calm. Act wisely.
Cyndy Gregoria
15 Dec, 2025
You got this. I was in your shoes two years ago. My aneurysm was 5.2mm, and I thought I was going to die. I cried in the parking lot after my neurologist said "monitor." But then I started walking 30 minutes a day, swapped soda for water, and joined a support group. I didn’t fix my aneurysm - I fixed my life. And now? I’m hiking, traveling, and laughing more than ever. You’re not a patient. You’re a person. And you’re stronger than you think.
Justin Hampton
15 Dec, 2025
Everyone’s acting like this is some groundbreaking article. Newsflash: we’ve known all this since the 90s. The real story is how little has changed. We still use PHASES. We still use coils and clips. We still don’t have a blood test. We still don’t know why some people get them and others don’t. This isn’t science - it’s repetition with fancy charts. Meanwhile, people are still dying because hospitals can’t afford flow diverters. So yeah. Thanks for the recap. Now go fix the system.