Running out of your blood pressure or diabetes meds because you forgot to refill them? You’re not alone. Most people on long-term medication refill their prescriptions every 30 days - that’s 12 trips to the pharmacy a year. But what if you could cut that down to just four? It’s possible, and it’s not complicated. All you need is to ask for a 90-day supply of your maintenance medications.
What Is a 90-Day Supply, and Why Does It Matter?
A 90-day supply means getting three months’ worth of your regular medication in one go. Instead of picking up your pills every month, you get them delivered or picked up once every three months. This isn’t just about saving time. Studies show people who use 90-day supplies are 27% more likely to take their meds as prescribed. That’s huge. Missing doses can lead to hospital visits, worsening conditions, and higher costs down the line. These programs work best for chronic conditions - things you take every day, long-term. Think high blood pressure, cholesterol, diabetes, thyroid meds, depression, or asthma inhalers. They don’t work for short-term drugs like antibiotics or painkillers after surgery. Your insurance and pharmacy benefit manager (PBM) set the rules, but the goal is simple: make it easier to stay on track.Check If Your Insurance Covers It
Not every plan offers 90-day supplies, and not all pharmacies handle them the same way. Start by checking your insurance website or calling the member services number on your card. Look for terms like:- 90-day supply
- Mail-order pharmacy
- Extended-day supply
- CVS Caremark, Express Scripts, Cigna 90 Now, Aetna
Make Sure Your Medication Qualifies
Your doctor can’t just write a 90-day script for anything. Insurance companies and pharmacies have lists of approved medications. These are called “maintenance drugs.” Here’s what qualifies:- Drugs taken daily for chronic conditions
- Generic versions are usually preferred (and cheaper)
- Not controlled substances or short-term meds
Get Your Doctor on Board
This is the step most people skip. Your doctor may automatically write a 30-day script because that’s what they’ve always done. You need to ask them to change it. Say something simple: “I’d like to switch to a 90-day supply for my [medication name]. It would help me stay on track and reduce trips to the pharmacy.” Most doctors are happy to help - especially if you explain it’s about adherence. Some even have pre-written templates for this. You have two options to get the prescription:- Ask your doctor to send an electronic 90-day prescription directly to your mail-order pharmacy (like CVS Caremark or Express Scripts). This is the fastest way.
- Ask your pharmacy to contact your doctor on your behalf. They’ll call, explain the request, and get approval. This can take a few extra days.
Choose Your Delivery Method
Once your prescription is approved, you’ve got choices:- Mail-order pharmacy: Most common. CVS Caremark, Express Scripts, and Aetna send meds directly to your door. Delivery usually takes 7-10 business days. Some offer free shipping and refill reminders.
- Select retail pharmacies: Cigna 90 Now and Walmart let you get 90-day fills at certain locations. Walmart’s generic drugs cost just $10 for 90 days - no insurance needed. But you must use their network pharmacies.
- Specialty pharmacies: For complex meds, you may need to use a dedicated specialty pharmacy that handles storage and delivery.
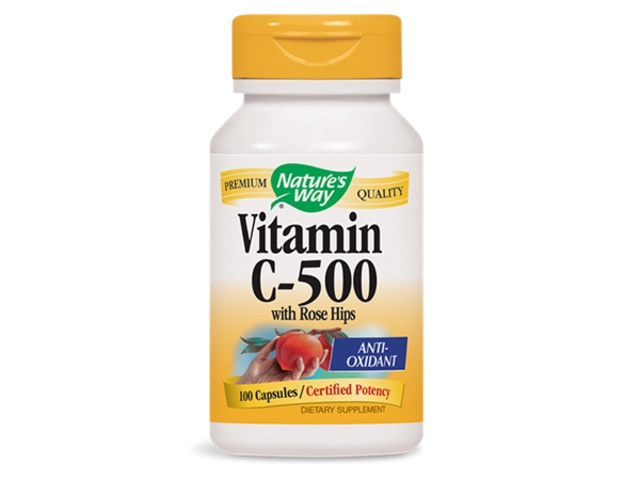
Understand the Cost Differences
The big win? Lower out-of-pocket costs. On average, people save $2.35 per prescription each month by switching to 90-day supplies. That’s about $28 a year per med. For someone on three meds? That’s $84 saved annually - and you’re not even trying. Here’s how pricing usually breaks down:| Medication Type | Mail-Order (e.g., Express Scripts) | Walmart (Retail) | Generic vs. Brand |
|---|---|---|---|
| Generic (e.g., Lisinopril) | $10-$20 | $10 | Lowest cost |
| Preferred Brand (e.g., Lipitor) | $20-$40 | $70-$100 | Mail-order usually cheaper |
| Non-Preferred Brand | $40-$140 | $100+ | Significant savings with mail-order |

Watch Out for Common Pitfalls
Even with all the benefits, things can go wrong. Here’s what to avoid:- Assuming all pharmacies offer it. Not every CVS or Walgreens does. Check your plan’s network.
- Forgetting to renew. Set a calendar reminder for 75 days in - that way, you’re not scrambling if delivery is late.
- Trying to use it for acute meds. Antibiotics, steroids, or pain meds won’t qualify. Stick to daily maintenance drugs.
- Living in a restricted state. Some programs aren’t available in California, Minnesota, New Hampshire, Texas, or Washington. Check your plan’s terms.
- Not checking for drug interactions. Mail-order pharmacies now offer safety checks. Use them. Call if you start a new med.
What If It Doesn’t Work?
Sometimes, your plan won’t allow it. Your doctor refuses. Your med isn’t covered. Here’s what to do:- Ask your pharmacy to file an exception request with your insurer.
- Call your insurance company’s appeals line. Sometimes, they’ll approve it if you explain your adherence history.
- Switch to a different plan during open enrollment if this is a recurring issue.
- Use Walmart’s $10 generic program - no insurance needed.
Start Today - One Step at a Time
You don’t need to fix everything at once. Pick one medication. Check your plan. Call your doctor. Ask for the 90-day script. In a few weeks, you’ll have fewer trips, fewer missed doses, and more peace of mind. The goal isn’t perfection. It’s consistency. And a 90-day supply is one of the easiest, most proven ways to get there.Can I get a 90-day supply of my birth control pills?
Yes. Many insurance plans allow 84-day supplies (three packs) of oral contraceptives, which count as a 90-day supply under most pharmacy benefit programs. You’ll still get the same benefits: fewer trips, lower cost, and better adherence. Just ask your doctor to write the script for 84 days or 90 days, depending on your plan’s rules.
Do I need to change pharmacies to get a 90-day supply?
It depends. If you want mail-order delivery, you’ll need to use your plan’s designated pharmacy like CVS Caremark or Express Scripts. If you prefer to pick it up, you can use select retail pharmacies - but only those in your plan’s network. For example, Cigna 90 Now only works at certain CVS or Walgreens locations. Check your plan’s website or call customer service to find approved pharmacies near you.
Can I get 90-day supplies if I’m on Medicare?
Yes. Medicare Part D plans are required to offer 90-day supply options for maintenance medications. Medicare Advantage plans (Part C) often go further, offering 100-day supplies. You can choose mail-order or select retail pharmacies. Just make sure your specific plan includes the benefit - some low-cost plans have restrictions. Call your plan’s member services to confirm.
What if my doctor won’t write a 90-day prescription?
Some doctors aren’t familiar with the process or worry about liability. Politely explain that studies show 90-day supplies improve adherence by 27% and reduce hospitalizations. Offer to print out a fact sheet from your insurer or the CDC. Many doctors will agree once they understand the benefits. If they still refuse, ask if they’ll let your pharmacy contact them to explain.
Are there any medications that can’t be filled for 90 days?
Yes. Short-term medications like antibiotics, painkillers, or steroids usually can’t be filled for 90 days. Specialty drugs for conditions like cancer or MS often require three 30-day fills before switching. Some states restrict certain drugs. Always check your plan’s formulary list or call customer service to confirm eligibility before assuming.








Anastasia Novak
6 Jan, 2026
Okay but let’s be real - if you’re not using mail-order for your 90-day scripts, you’re literally leaving free money on the table. I’ve been on lisinopril for 7 years and my copay went from $45 to $8. That’s not savings, that’s a heist. Also, CVS Caremark sends you a little card with your meds that says ‘You got this.’ I cried. Not because I’m weak - because corporate empathy is weirdly effective.
Elen Pihlap
6 Jan, 2026
OMG YES I DID THIS AND MY HUSBAND SAID I’M TOO LAZY TO GO TO THE PHARMACY BUT I’M NOT LAZY I’M SMART AND I SAVE TIME AND NOW I HAVE TIME TO WATCH NETFLIX AND NOT THINK ABOUT MY DIABETES
Sai Ganesh
7 Jan, 2026
In India, we have a similar system called ‘chronic disease management’ under government schemes. Many pharmacies offer 90-day supplies at half the cost, especially for hypertension and diabetes. The real challenge isn’t access - it’s awareness. People still think ‘doctor writes 30 days’ means ‘only 30 days allowed.’ Education matters more than policy.
Paul Mason
8 Jan, 2026
Look, I’ve been doing this since 2018. 90-day scripts are the only reason I haven’t ended up in A&E. People act like it’s some big secret. It’s not. It’s basic. If you’re on meds longer than a cold, you deserve this. Also, Walmart’s $10 generics? That’s not a deal - that’s a public service. Shame on insurers who make you jump through hoops.
Katrina Morris
8 Jan, 2026
i just switched my metformin to 90 days and now i dont forget to take it like i used to and also my cat likes to sit on the pill organizer so its cute now
also i think the mail order guy knows my name now and he waved at me through the window when he dropped it off lol
Anthony Capunong
9 Jan, 2026
Why are we letting corporations dictate how we get our medicine? This isn’t convenience - it’s control. Mail-order means they track you. They know your habits. They know your health. And they sell that data. You think this is about saving money? No. It’s about surveillance capitalism wrapped in a wellness bow.
Kyle King
11 Jan, 2026
They’re not giving you 90-day supplies because they care. They’re doing it because they’re trying to make you dependent. Next thing you know, they’ll be mailing your oxygen tanks and your insulin with a QR code that links to a survey about your emotional state. This is Step 1 of the Great Pharma Takeover. Wake up.
Emma Addison Thomas
12 Jan, 2026
I appreciate the practical advice, especially about checking your plan’s network. In the UK, we don’t have mail-order pharmacies per se, but we do get 3-month prescriptions through the NHS - and they’re free. It’s not perfect, but it removes the stress of refills. Maybe the US system could learn something from simpler models.
Rachel Steward
13 Jan, 2026
Let’s deconstruct this. The 27% adherence increase? Correlation isn’t causation. People who seek 90-day supplies are already more health-literate. The study likely suffers from selection bias. Also, the $2.35 monthly savings? That’s negligible when you consider the hidden costs: delayed access, shipping errors, expired meds sitting in your drawer for 80 days, and the psychological toll of ‘out of sight, out of mind.’
And let’s not ignore the structural flaw - this system rewards passive compliance, not active health management. Are we optimizing for convenience or for autonomy? Because this feels like corporate wellness theater dressed up as empowerment.
Jonathan Larson
14 Jan, 2026
It is a profound and often underappreciated truth that human health is not merely a biological phenomenon, but a deeply relational one. The act of requesting a 90-day supply is not simply logistical - it is an assertion of dignity, of responsibility, of self-advocacy in a system designed to depersonalize care. One does not merely ‘get a prescription’ - one engages in a quiet act of resistance against fragmentation, against forgetfulness, against the erosion of continuity in an age of distraction.
When we choose to consolidate care, we choose to honor the sacred rhythm of healing. The pharmacy becomes not a transactional node, but a pillar of stability. And in that stability, we find not just adherence - but peace.
Alex Danner
14 Jan, 2026
Pro tip: if your doctor says ‘I don’t write 90-day scripts,’ hand them this link to your insurer’s formulary page. Most docs don’t know the rules - they just copy-paste 30-day scripts out of habit. I had to show mine a screenshot of my plan’s coverage page. He said ‘Oh. I didn’t know that was an option.’
Also, if you’re on Medicare, don’t forget to ask about the 100-day option. That’s 3+ months. You’ll thank me later.
LALITA KUDIYA
14 Jan, 2026
in india we use 90 day supplies too for diabetes and bp
but we dont have mail order so we ask pharmacy to keep stock
and they give us 1 month at a time but with extra 10 pills for free
its not perfect but its working
also i use whatsapp reminder for refill
thank you for this post it made me feel less alone
Aparna karwande
16 Jan, 2026
How dare you normalize dependency on Big Pharma’s convenience traps? You think this is progress? This is surrender. In my country, we don’t let corporations decide how often we take our medicine. We take responsibility. We refill. We show up. We don’t outsource our health to a drone delivery service because we’re too ‘busy.’ This isn’t empowerment - it’s corporate laziness disguised as innovation.
Jessie Ann Lambrecht
17 Jan, 2026
I switched my birth control to 84-day and now I don’t have to panic every month when I’m out of town. I once missed a refill and ended up in the ER with a panic attack because I thought I was pregnant - turns out I just forgot. Now? I set a calendar alert for Day 75 and I’m golden.
Also - Walmart’s $10 lisinopril? I’ve been buying it for my mom who doesn’t have insurance. She calls it her ‘magic pill.’ I call it a miracle.
Vince Nairn
17 Jan, 2026
Wow. So we’re celebrating corporate efficiency now? Next thing you know, we’ll be getting our antidepressants in bulk with a coupon for a free meditation app.
Meanwhile, I’m still paying $120 for my 30-day script at CVS because my plan ‘doesn’t cover mail-order.’ So thanks for the feel-good article about a system that doesn’t work for most people.