What Is Hepatic Encephalopathy?
Hepatic encephalopathy (HE) isn’t a disease on its own-it’s your brain reacting to a failing liver. When your liver can’t clean out toxins, especially ammonia, those toxins slip into your bloodstream and reach your brain. This causes confusion, memory lapses, personality shifts, and in severe cases, coma. It’s not dementia. It’s not Alzheimer’s. It’s your liver screaming for help, and your brain is the one paying the price.
People with cirrhosis are most at risk. About 3 in 10 will have a clear episode of HE at some point. But up to 8 in 10 may have tiny, invisible changes in thinking-called minimal HE-that only show up on special tests. These aren’t just "getting older." They’re signs your liver isn’t keeping up.
Why Does Confusion Happen?
The main culprit is ammonia. Your gut makes it when bacteria break down protein. A healthy liver traps it and turns it into urea, which you pee out. But when the liver is damaged, ammonia bypasses it. It flows straight to your brain through abnormal blood vessels called shunts.
In the brain, ammonia makes brain cells swell, messes with neurotransmitters, and causes oxidative stress. That’s why people with HE feel foggy, sleepy, or irritable. They might forget names, mix up days, or suddenly act out of character. In advanced stages, speech becomes slurred, they can’t focus, and they may slip into coma.
Ammonia levels don’t always match symptoms. Someone with a level of 80 μmol/L might feel fine, while another with 60 μmol/L is confused. That’s why doctors don’t rely on blood tests alone. They look at your liver function, your behavior, and what’s happened recently.
What Triggers a Hepatic Encephalopathy Episode?
HE doesn’t come out of nowhere. Something pushes your liver over the edge. The most common triggers:
- Infections-especially spontaneous bacterial peritonitis (SBP), which causes 25-30% of HE episodes.
- Bleeding in the gut-from ulcers or varices. Blood in the intestines becomes protein that bacteria turn into ammonia.
- Electrolyte imbalances-low potassium or sodium from diuretics or vomiting.
- Constipation-letting waste sit means more time for gut bacteria to make ammonia.
- Sedatives and painkillers-benzodiazepines (like Valium) can make HE worse by 3.2 times.
- Dehydration-low blood volume makes it harder for your body to flush out toxins.
One patient on a liver forum tracked his episodes for months and realized every flare-up came after a urinary tract infection. He started testing monthly-and cut his HE episodes by 80%. Small triggers, big impact.
How Lactulose Works-And Why It’s Still the First Line
Lactulose has been the go-to treatment since 1966. It’s not a drug that kills bacteria. It’s a sugar your body can’t digest. When it reaches your colon, gut bacteria break it down. This acidifies your gut-lowering the pH from 7 to about 5.5.
Here’s the key: ammonia (NH₃) is a gas that can slip into your bloodstream. But when the gut is acidic, ammonia turns into ammonium (NH₄⁺), which can’t cross into your blood. It gets trapped and flushed out with your stool.
Doctors usually start with 30-45 mL, taken 3-4 times a day. The goal? Two to three soft stools daily. Not diarrhea. Not constipation. Just right.
But here’s the problem: 65% of people who don’t respond to lactulose are just not taking enough. They’re on 15 mL a day when they need 90 mL. Others stop because of the taste-it’s sweet and syrupy, like cough medicine gone wrong. Or they get cramps and diarrhea and think it’s too much.
Some take it rectally as an enema if they’re too confused to swallow. A 300 mL dose diluted in water can work fast-within hours.
Rifaximin: The Second Line That Makes a Difference
If lactulose alone isn’t enough, doctors add rifaximin. It’s an antibiotic that doesn’t get absorbed into your blood. It stays in your gut and kills the ammonia-making bacteria-especially Klebsiella and Proteus.
The RIFHE study showed rifaximin cuts recurrent HE episodes by 58% compared to placebo. It’s taken as 550 mg twice daily. It’s expensive-about $1,200 a month-but for many, it’s life-changing.
One patient on Hep Forums said: "After six months of lactulose and rifaximin, my cognitive scores improved. I went from barely able to read to working part-time again."
But it’s not perfect. There’s a small risk of C. diff infection (0.2%), and some gut bacteria are starting to resist it. That’s why doctors don’t use it alone-it’s always paired with lactulose.
What About Diet? Should You Cut Protein?
For decades, doctors told people with HE to eat less protein. That’s outdated.
Current guidelines say: during an acute HE episode, cut protein to 0.5 grams per kilogram of body weight for a few days. But once you’re stable, go back to 1.2-1.5 grams per kg. That’s about 70-90 grams a day for most adults.
Why? Muscle loss from too little protein makes your liver work harder. Protein helps repair tissue. The key isn’t cutting it-it’s spreading it out. Eat small amounts throughout the day. Choose plant-based proteins like beans and lentils when possible-they make less ammonia than red meat.
Also, avoid alcohol completely. Even small amounts can trigger HE. And skip sedatives, sleeping pills, and OTC painkillers like ibuprofen if you have cirrhosis.
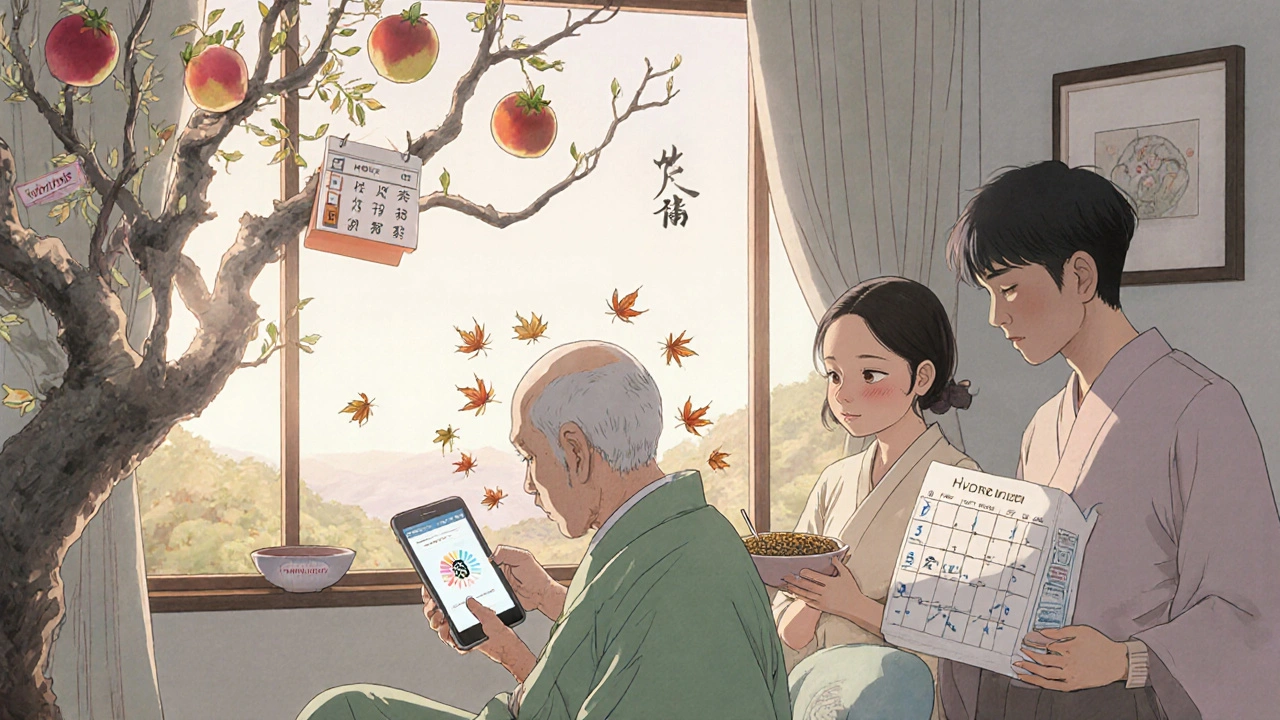
How to Prevent Hepatic Encephalopathy
Prevention beats treatment every time. Here’s what works:
- Take lactulose daily if you’ve had HE before-even when you feel fine. Prophylactic dosing (15 mL twice daily) cuts recurrence by 50% in six months.
- Stay regular-constipation is a silent trigger. Use stool softeners if needed. Walk daily. Drink water.
- Watch for infections-fever, chills, belly pain? Get checked fast. UTIs, pneumonia, and even dental infections can spark HE.
- Track your symptoms-keep a simple log: mood changes, sleep patterns, confusion, handwriting quality. Family members often spot changes before doctors do.
- Use the EncephalApp-a free smartphone app that tests your reaction time and attention. It’s used in clinics to catch minimal HE early.
- Get vaccinated-hepatitis A and B vaccines prevent further liver damage.
One study found that patients who tracked their symptoms and had regular check-ins with a nurse had 40% fewer hospital visits.
What Happens If It’s Not Treated?
Untreated HE doesn’t just cause confusion-it kills. About 25-30% of people who go into coma from acute HE don’t survive. Even if they do, they often need long-term care.
And the costs? A single hospital admission for HE runs about $28,500. Outpatient management with lactulose? Around $1,200 a year. Preventing one episode saves over $14,000.
HE is one of the most expensive complications of liver disease in the U.S.-$1.1 billion a year. But it’s also one of the most preventable.
What’s New in HE Treatment?
The field is changing fast. In 2023, the FDA approved a new combo pill called Xifaxilac-lactulose and rifaximin in one tablet. It’s easier to take. More people will stick with it.
Another promising option is AST-120, an oral adsorbent approved in Japan since 2005. It soaks up toxins in the gut before they’re absorbed. Early results show it lowers ammonia and improves thinking.
Fecal microbiota transplants (FMT) are being tested for refractory HE. In one trial, 70% of patients saw ammonia levels drop after FMT. It’s not standard yet-but it’s coming.
And researchers are developing a blood test that predicts HE risk with 85% accuracy using 12 biomarkers. That could change everything-catching problems before symptoms start.
When to Call for Help
If you or someone you care for has liver disease and starts showing these signs:
- Forgetfulness that’s getting worse
- Slurred speech or trouble forming words
- Personality changes-aggression, apathy, or extreme sleepiness
- Hand tremors or flapping movements (asterixis)
- Confusion about time, place, or people
Don’t wait. Call your liver specialist or go to the ER. Early treatment can reverse HE. Delayed treatment can cost you your life.
Final Thought: It’s Manageable
Hepatic encephalopathy isn’t a death sentence. It’s a signal. Your liver is struggling. But with the right tools-lactulose, rifaximin, good habits, and early detection-you can live well. Many people return to work, drive, and enjoy time with family. It takes effort. It takes consistency. But it’s possible.
Is hepatic encephalopathy reversible?
Yes, in most cases. If caught early and treated properly, HE can fully reverse. Many patients regain normal thinking and function after starting lactulose and addressing triggers like infection or constipation. But if HE progresses to coma or is left untreated, brain damage can become permanent. Speed matters.
Can you take lactulose long-term?
Absolutely. Lactulose is safe for long-term use. Many people take it daily for years to prevent HE recurrence. Side effects like bloating or cramps usually improve after a few weeks. If diarrhea is severe, your doctor can lower the dose. It’s not addictive and doesn’t harm the kidneys or liver.
Does ammonia testing help diagnose HE?
Not reliably in chronic liver disease. Ammonia levels don’t always match symptoms. Someone with a high level might feel fine, while someone with a normal level is confused. Doctors rely more on clinical signs, liver function tests, and ruling out other causes. Ammonia tests are most useful in acute liver failure, not cirrhosis.
Why do some people with HE get worse on antibiotics?
Rifaximin is designed to work only in the gut and doesn’t cause systemic issues. But other antibiotics can disrupt the gut microbiome in unpredictable ways. Some kill good bacteria that help control ammonia, while others may promote resistant strains. That’s why rifaximin is preferred-it’s targeted. Never take random antibiotics without talking to your liver specialist.
Can lifestyle changes prevent HE?
Yes, and they’re essential. Staying hydrated, avoiding alcohol, managing constipation, eating balanced protein, and taking lactulose as prescribed can prevent 80% of episodes. Regular walks, checking for infections early, and tracking symptoms with a journal make a huge difference. Prevention isn’t optional-it’s the foundation of living well with cirrhosis.









Aishwarya Sivaraj
27 Nov, 2025
I've been managing HE for my mom for 3 years now and lactulose was a game changer
She used to get so confused after eating red meat, now she eats lentils and beans and barely blinks
Constipation is the silent killer here, and walking 20 mins a day does more than any pill
Iives Perl
28 Nov, 2025
Lactulose is a government mind control drug lol
They don't want you to know the real cure is apple cider vinegar + colloidal silver 🤫💊
steve stofelano, jr.
28 Nov, 2025
The clinical evidence supporting lactulose as a first-line intervention for hepatic encephalopathy remains robust and is endorsed by the American Association for the Study of Liver Diseases. Furthermore, the integration of rifaximin as an adjunctive therapy demonstrates a statistically significant reduction in recurrence rates, as validated by the RIFHE trial. Preventive strategies, including meticulous bowel regimen management and early infection detection, constitute the cornerstone of long-term patient outcomes.
Savakrit Singh
29 Nov, 2025
Lactulose is just a placebo wrapped in syrup 🤡
Big Pharma doesn't want you to know that FMT has a 70% success rate and costs $500
Why are we still using 1960s sugar water when we have microbiome tech? 🧬💸
Also, your 'minimal HE' stats? They're inflated. The real numbers are buried in NIH grant reports. #LiverTruth
Cecily Bogsprocket
30 Nov, 2025
I used to think my dad was just getting forgetful with age
Then he started mixing up my name and calling me by his sister’s
We started him on lactulose and within a week he remembered my birthday
It’s not magic, it’s just science that actually works
Don’t wait until he can’t tie his shoes
Trust me, I’ve been there
Jebari Lewis
30 Nov, 2025
The fact that we still treat HE like it's a mystery is criminal
Ammonia? Lactulose? Rifaximin? We've had this for decades
Yet people still die because they're not taking enough lactulose because the doctor didn't explain it properly
Education is the real gap, not medication
And yes, I've seen patients reverse cognitive decline after 6 months of consistent treatment
It's not a miracle - it's responsibility
Emma louise
1 Dec, 2025
Oh great, another 'liver expert' telling us to take syrup and eat beans
Meanwhile, real doctors are using IV glutathione and ozone therapy
But no, let's just keep feeding people sugar water and call it medicine 🙄
sharicka holloway
2 Dec, 2025
I work with liver patients every day and I’ve seen people come back from coma
It’s not about being perfect - it’s about showing up
Even if you forget to take lactulose one day, just take it the next
Don’t shame yourself, just keep going
You’re not failing - you’re fighting