Atazanavir CNS Risk Estimator
This tool helps assess your potential risk of neurological side effects while taking Atazanavir based on your current health factors. Remember, this is not a diagnostic tool and should not replace professional medical advice.
Quick Takeaways
- Atazanavir is an HIV protease inhibitor that can increase bilirubin levels, sometimes leading to mild jaundice.
- It crosses the blood‑brain barrier only in small amounts, so direct neurotoxicity is rare.
- Reported CNS side effects include headache, insomnia, and occasional mood changes.
- Some studies suggest a protective effect against HIV‑associated neurocognitive disorder because of strong viral suppression.
- Monitoring bilirubin, drug interactions, and patient‑reported symptoms helps keep risks low.
When you hear a drug name paired with “brain,” you might expect big safety warnings or even a miracle cure. With Atazanavir is a once‑daily HIV protease inhibitor used in antiretroviral therapy (ART), the reality sits somewhere in the middle. Clinicians and patients alike wonder whether the medication can harm the central nervous system (CNS) or, conversely, help protect it from HIV‑related damage. This guide unpacks the chemistry, the clinical data, and the practical steps you can take to balance potential risks and benefits.
How Atazanavir Works - The Pharmacology Basics
Atazanavir belongs to the protease inhibitor class, which blocks the HIV‑1 protease enzyme, preventing the virus from maturing into an infectious form. By halting viral replication, it reduces the viral load in blood, lymph, and-importantly-cerebrospinal fluid (CSF). The drug is typically boosted with a low dose of ritonavir (a strong CYP3A4 inhibitor) to boost plasma concentrations. This boosting strategy improves efficacy but also raises the chance of drug‑drug interactions.
Does Atazanavir Reach the Brain?
The blood‑brain barrier (BBB) is a selective wall that protects the CNS from toxins and many medications. Atazanavir’s ability to cross the BBB is limited because it is a relatively large, lipophilic molecule and a substrate for efflux pumps like P‑glycoprotein. Studies measuring CSF concentrations show that at steady‑state, atazanavir levels in CSF are roughly 1‑2% of plasma levels, well below the IC50 needed to inhibit HIV in the CNS.
However, even low concentrations matter if the drug’s presence suppresses HIV replication in the brain. Effective viral suppression reduces the risk of HIV‑associated neurocognitive disorder (HAND), which is a major concern for people living with HIV.
Potential Neurological Risks
While atazanavir is not a classic neurotoxin, certain side effects can indirectly affect brain health:
- Hyperbilirubinemia: Atazanavir inhibits UDP‑glucuronosyltransferase 1A1, causing indirect bilirubin to rise. Elevated bilirubin can cause mild jaundice and, in rare cases, contribute to fatigue or light‑sensitivity, which may exacerbate headache or concentration issues.
- Headache and Dizziness: Reported in 5‑10% of patients, often transient and manageable with hydration and caffeine.
- Sleep Disturbances: Insomnia or vivid dreams have popped up in clinical trial safety data; the mechanism is unclear but may involve CNS penetration of the boosted regimen.
- Mood Changes: A handful of case reports link atazanavir to depression or irritability, usually reversible after dose adjustment or discontinuation.
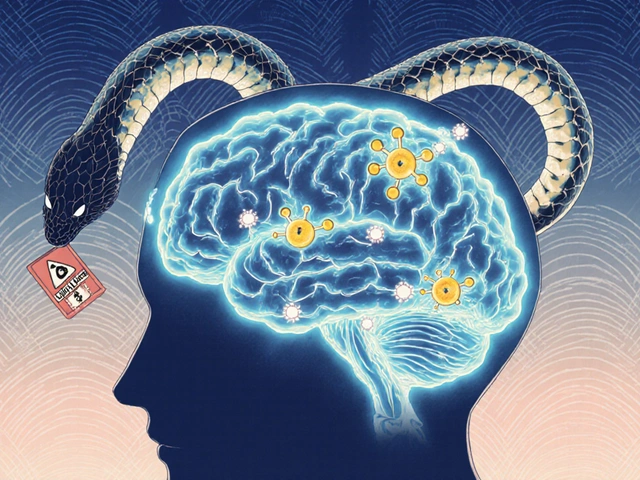
- Drug‑Drug Interactions: Because atazanavir/ritonavir blocks CYP3A4, co‑administration with sedatives, antiepileptics, or psychiatric meds can raise or lower their levels, indirectly influencing cognition or mood.
It’s worth noting that severe neurotoxicity-like seizures or encephalopathy-has not been linked to atazanavir in large cohorts. Most CNS complaints are mild, short‑lived, and often improve with supportive care.
Documented Benefits for the Brain
The flip side is that strong viral suppression can protect the brain. HAND affects up to 50% of untreated HIV patients, ranging from asymptomatic neurocognitive impairment to HIV‑associated dementia. By keeping plasma and CSF viral loads below detection, atazanavir helps:
- Prevent new neuronal injury caused by HIV proteins (e.g., gp120, Tat).
- Reduce inflammatory cytokine release in the CNS.
- Stabilize neurocognitive test scores over years, as shown in the ACTG 5257 trial where atazanavir‑ritonavir performed comparably to darunavir‑ritonavir in preserving cognitive function.
Additionally, the drug’s favorable lipid profile (it tends to lower triglycerides compared with some older PIs) may indirectly support vascular health, another key factor for brain aging.
Clinical Evidence - What the Studies Say
Below is a side‑by‑side look at three major protease inhibitors and their reported CNS side effects. Data are drawn from phase III trials, post‑marketing surveillance, and meta‑analyses up to 2024.
| Drug | BBB Penetration (CSF % of plasma) | Common CNS AEs | Serious CNS AEs |
|---|---|---|---|
| Atazanavir/ritonavir | ~1-2 % | Headache, insomnia, mild mood changes | None reported in >10,000 pts |
| Lopinavir/ritonavir | ~3 % | Dizziness, vivid dreams | Rare seizures (<0.1 %) |
| Darunavir/ritonavir | ~2 % | Fatigue, headache | Isolated cases of encephalopathy (<0.05 %) |
Notice that the incidence of serious CNS events stays under 0.1 % for all three drugs, underscoring that major neurotoxicity is exceptionally rare when patients adhere to prescribed regimens.
Managing Risks - Practical Tips for Clinicians and Patients
- Baseline Assessment: Before starting atazanavir, obtain a thorough neurocognitive screen (e.g., Montreal Cognitive Assessment) and check bilirubin levels.
- Monitor Bilirubin: Repeat total and direct bilirubin at weeks 4, 12, and then every six months. If indirect bilirubin exceeds 3 mg/dL and causes symptomatic jaundice, consider dose reduction or switch to a non‑boosted regimen.
- Drug Interaction Review: Use a reliable interaction checker for any concurrent CNS‑active agents (e.g., benzodiazepines, antipsychotics). Adjust doses or choose alternative ART when needed.
- Symptom Tracking: Encourage patients to log headaches, sleep quality, and mood changes in a simple diary. Patterns often emerge that guide preventive measures.
- Address Sleep Issues: Simple measures-limit caffeine after noon, maintain a regular bedtime, and avoid screen exposure-can reduce insomnia linked to atazanavir.
- Switch Strategy: If CNS side effects persist beyond four weeks despite supportive care, discuss switching to another protease inhibitor or an integrase strand transfer inhibitor (INSTI), which generally have even lower CNS penetration.
These steps keep the atazanavir brain effects under a manageable level while preserving the drug’s antiviral power.

Checklist - Quick Reference for Everyday Use
- ✅ Confirm HIV viral load is < 50 copies/mL before initiating atazanavir.
- ✅ Record baseline bilirubin (aim for < 1 mg/dL).
- ✅ Review all current meds for CYP3A4 interactions.
- ✅ Schedule neurocognitive assessment at 3‑month intervals.
- ✅ Educate patient about possible headache, insomnia, and mild jaundice.
- ✅ Have a plan for fast switch if serious CNS AEs develop.
Future Directions - What Researchers Are Eyeing
Newer formulations aim to reduce ritonavir boosting, which could lower interaction risk. Long‑acting injectable depots of protease inhibitors are in Phase II trials; if successful, they might eliminate daily pill burden and associated CNS complaints like insomnia linked to nocturnal dosing.
Another hot topic is neuro‑protective adjuncts-like memantine or anti‑inflammatory agents-to pair with ART and further shield the brain from HIV‑related inflammation. While data are early, ongoing studies in 2025 are testing whether adding low‑dose minocycline improves cognitive scores in patients on atazanavir.
Frequently Asked Questions
Can Atazanavir cause permanent brain damage?
No. Large safety databases involving tens of thousands of patients have not linked atazanavir to permanent neurodegeneration. Most CNS symptoms are mild, reversible, and resolve after dose adjustment or discontinuation.
Why does Atazanavir raise bilirubin?
Atazanavir inhibits the enzyme UDP‑glucuronosyltransferase 1A1, which normally converts indirect (unconjugated) bilirubin into a water‑soluble form. The blockage leads to a buildup of indirect bilirubin, causing a harmless jaundice in most people.
Is the brain‑protective effect of Atazanavir proven?
Direct neuroprotection isn’t the primary goal, but strong viral suppression-shown in multiple trials-reduces HIV‑related inflammation in the CNS, which indirectly protects cognitive function.
Should I avoid caffeine while on Atazanavir?
Caffeine isn’t a known interaction, but if you experience headaches or insomnia, cutting back on caffeine after noon can help.
How often should I get my bilirubin checked?
Check at baseline, then at 4 weeks, 12 weeks, and every six months thereafter, unless you develop visible jaundice or symptoms that warrant earlier testing.
Understanding the balance between risk and benefit empowers you to make informed choices about atazanavir therapy. By staying vigilant, monitoring key labs, and communicating openly with your healthcare team, you can enjoy the drug’s antiviral strength while keeping your brain safe and sharp.







Harini Prakash
22 Oct, 2025
I really appreciate the thorough breakdown you gave on atazanavir and its relationship with the brain :)
It’s reassuring to see the emphasis on both the potential risks and the protective benefits.
The point about hyperbilirubinemia causing mild fatigue and light‑sensitivity is spot on, because many patients notice those subtle changes before anything serious occurs.
I also like how you highlighted that the drug’s CSF concentrations are only 1‑2% of plasma levels, which helps explain why direct neurotoxicity is rare.
Your mention of the ACTG 5257 trial provides solid evidence that cognitive function can be preserved with proper viral suppression.
It’s useful to remember that the BBB limits the drug’s penetration, yet even low levels can still contribute to keeping HIV out of the CNS.
The discussion on drug‑drug interactions with CYP3A4 was clear, and it reminds clinicians to review psychiatric meds carefully.
I’ve seen patients who experience occasional insomnia, and a simple hydration strategy often helps mitigate the headache component.
Your note on the favorable lipid profile of atazanavir compared to older PIs is a nice bonus for vascular brain health.
Overall, I think the balanced view you provided can guide both providers and patients in making informed choices.
If anyone is starting therapy, regular monitoring of bilirubin and symptom logs will catch the mild side effects early.
In practice, I’ve found that a supportive coaching approach-checking in weekly-helps patients feel empowered to report any new CNS symptoms.
Keep spreading this kind of nuanced information; it helps demystify the medication and reduces unnecessary fear.
Thank you for the clear, empathetic tone throughout the article! 😊
Rachael Turner
4 Nov, 2025
Your summary reminds me how medicine is a bridge between chemistry and lived experience. We see data and then we see how it feels in day to day life. The brain is fragile yet resilient and drugs like atazanavir tip the balance in subtle ways. It is comforting that the risks are modest but we must stay vigilant.
Kiara Gerardino
17 Nov, 2025
It is utterly scandalous that anyone would downplay the moral responsibility of prescribing a drug with even the slightest chance of neuropsychiatric harm! The pharmaceutical industry peddles hope while hiding the shadows of mood disturbances and insomnia, and we, as a society, must demand absolute transparency and ethical stewardship. No patient should be left to suffer vague side effects while the profit margins soar.
Tim Blümel
30 Nov, 2025
I hear your passion and it sparks an important dialogue 😌. While the stakes are high, we also need to weigh the undeniable protective benefits against HIV‑associated neurocognitive decline. A balanced perspective, grounded in robust data, can guide us to use atazanavir responsibly while safeguarding mental health.
Joanne Ponnappa
13 Dec, 2025
Atazanavir seems to have a low risk of serious brain issues, which is reassuring for many users.
Emily Collins
26 Dec, 2025
I must interject here – I’ve personally watched a friend battle severe insomnia after starting the regimen, and it was a nightmare that almost drove them to quit treatment. The drama of sleepless nights can’t be ignored, even if it’s “rare”. It’s crucial we don’t gloss over these hidden struggles.
Diane Thurman
7 Jan, 2026
This article is fine but it miss some key data.
Sarah Riley
20 Jan, 2026
The omission you note likely stems from selective reporting bias, a common pitfall in Phase III pharmacovigilance syntheses.