When you’re prescribed a medication to protect your bones from breaking, the last thing you expect is to hear about a rare but scary side effect: jaw necrosis. It sounds alarming. And it’s true - bisphosphonates, the most common drugs used to treat osteoporosis, have been linked to a condition called medication-related osteonecrosis of the jaw (MRONJ). But here’s the truth most people don’t hear: if you’re taking these pills for osteoporosis, your risk of developing this condition is extremely low - lower than being struck by lightning.
What Exactly Is MRONJ?
MRONJ isn’t just any jaw problem. It’s when the bone in your jaw becomes exposed and doesn’t heal for more than eight weeks. It can happen after a tooth extraction, gum surgery, or sometimes even without any obvious trigger. The jawbone loses its ability to repair itself because the medication shuts down the cells that normally break down and rebuild bone - osteoclasts. This is exactly what doctors want when treating osteoporosis: slow down bone loss. But in the jaw, where bone turns over ten times faster than in your hip or spine, this same mechanism can backfire.
It’s not caused by poor dental hygiene alone, but poor dental health combined with these drugs increases the risk. Think of it like this: if your gums are already inflamed or you have an infected tooth, and your body can’t heal properly because of the medication, the infection can spread to the bone. That’s when things get serious.
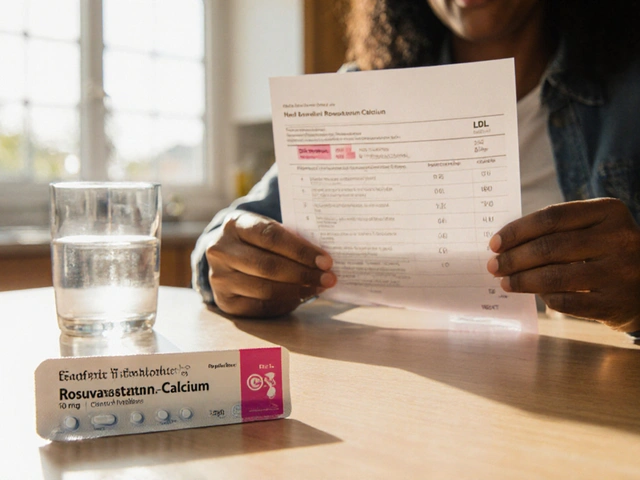
Bisphosphonates: The Good, the Bad, and the Misunderstood
Alendronate (Fosamax), risedronate (Actonel), and ibandronate (Boniva) are oral bisphosphonates. They’ve been around for decades. Since the 1990s, they’ve helped millions of older adults avoid broken hips and spinal fractures. The data is clear: alendronate cuts hip fracture risk by over 50% and spine fractures by nearly 50% over just a few years. That’s not a small win - it’s life-changing.
But here’s where the confusion starts. People hear “osteonecrosis of the jaw” and think it’s common. It’s not. For someone taking oral bisphosphonates for osteoporosis, the risk is about 0.7 cases per 100,000 people per year. That’s less than one in a hundred thousand. Compare that to cancer patients on high-dose IV bisphosphonates - their risk is 100 to 1,000 times higher. Why? Because they’re getting much stronger doses, often monthly, for years.
Even then, most cases happen in people who had dental work done while still on the drug - especially tooth extractions. A 2023 survey found that 63% of MRONJ cases in osteoporosis patients followed a dental extraction. That’s why dentists now ask: “Are you on osteoporosis meds?” before pulling a tooth.
Denosumab vs. Bisphosphonates: Which Is Riskier?
Denosumab (Prolia) is a newer drug, approved in 2010. It works differently - instead of targeting bone cells directly, it blocks a protein that activates them. It’s just as good at preventing fractures. But here’s the twist: multiple studies now show denosumab carries a higher risk of MRONJ than oral bisphosphonates. About 1.7 to 2.5 times higher. That’s not because it’s more dangerous overall - it’s because it works faster and more completely to stop bone turnover. And when you stop it, your bone can rebound quickly, which can lead to sudden, severe bone loss if you’ve had dental work.
That’s why doctors now advise: if you’re switching from bisphosphonates to denosumab, get your dental work done first. And if you’re coming off denosumab, wait at least three months before any major dental procedure.
Who’s Really at Risk?
Not everyone who takes these drugs will get MRONJ. In fact, most won’t. But certain factors raise the risk:
- Having gum disease, tooth decay, or loose teeth before starting the medication
- Getting invasive dental work - especially extractions - while on the drug
- Being on IV bisphosphonates (like zoledronic acid) for more than three years
- Smoking or having diabetes - both impair healing
- Using steroids long-term
Here’s something surprising: a 2011 study of 260,000 osteoporosis patients found no increased risk of jaw necrosis in those taking oral bisphosphonates compared to people not taking them at all. That’s right - the risk might be no higher than if you never took the drug. But if you have poor oral health? That’s when the numbers climb.

What Should You Do Before Starting or Continuing Treatment?
If you’ve been told you need bisphosphonates for osteoporosis, here’s your action plan:
- See your dentist before you start the medication. Get a full exam. Fix cavities, treat gum disease, remove teeth that are failing.
- Keep your teeth clean. Brush twice a day, floss daily. Use a soft-bristled brush if your gums are sensitive.
- See your dentist every six months. Even if you feel fine. Early signs of MRONJ - like a small piece of bone sticking out or a sore that won’t heal - are often painless at first.
- Tell your dentist you’re on bisphosphonates or denosumab. Don’t assume they know. Bring your prescription list.
- Avoid invasive procedures like implants or extractions unless absolutely necessary while on the drug.
If you’ve already been on bisphosphonates for years and haven’t had dental issues, don’t panic. The longer you’ve been on the drug without problems, the lower your risk becomes. The jawbone doesn’t suddenly turn to dust after five years - it’s a slow process tied to trauma and infection.
Drug Holidays: Do They Help?
Some doctors suggest stopping bisphosphonates for a few months before major dental work - a “drug holiday.” But it’s not simple. A major 2024 study found that stopping IV zoledronic acid for more than a year cuts MRONJ risk by 82%. But it also increases your fracture risk by 28%. That’s a huge trade-off.
For oral bisphosphonates, the data isn’t as clear. Most experts don’t recommend stopping them unless you’ve been on them for five years or more and have no other risk factors. The fracture protection lasts long after you stop taking the pill - sometimes for years - because the drug sticks to your bones. So stopping might not even help much.
Real Stories, Real Fears
One woman in Adelaide, 68, told her story online: after five years on alendronate, a routine cleaning revealed exposed bone. It took 18 months of antibiotics and surgery to heal. She’s now off the drug and says she’ll never go back.
Another man, 72, has been on Fosamax for 22 years. He’s had multiple extractions and two dental implants. Zero problems. His dentist says he’s the exception.
These stories aren’t contradictions - they’re reminders that risk isn’t the same for everyone. Your oral health, your lifestyle, your medical history - they all matter more than the drug name.
What’s Next?
The field is moving toward smarter treatment. Researchers are testing blood and urine markers to predict who’s at highest risk for MRONJ. In the next few years, we might see doctors use simple tests to decide: “You’re low risk - stay on bisphosphonates.” Or: “You’re high risk - switch to a different drug or take a break.”
For now, the message hasn’t changed: bisphosphonates save lives by preventing fractures. The risk of jaw necrosis is real - but it’s rare. And it’s almost always preventable with good dental care.
If you’re on one of these drugs and worried, talk to your doctor and your dentist together. Don’t stop the medication on your own. Don’t avoid the dentist out of fear. And don’t let a rare side effect scare you away from a treatment that could keep you walking, standing, and living without a broken hip.
Key Takeaways
- MRONJ is extremely rare in people taking oral bisphosphonates for osteoporosis - less than 1 in 100,000 per year.
- Denosumab carries a higher MRONJ risk than oral bisphosphonates, but both are far safer than the risk of a hip fracture.
- Most cases happen after dental extractions in people with existing gum disease or infection.
- Good oral hygiene and pre-treatment dental exams are the best way to prevent MRONJ.
- Stopping bisphosphonates to avoid MRONJ often increases fracture risk more than it reduces jaw problems.
Frequently Asked Questions
Can I still get dental implants if I’m on bisphosphonates?
Yes - but only if your dentist and doctor agree it’s safe. If you’ve been on oral bisphosphonates for less than three years and have healthy gums, implants are usually fine. If you’ve been on them longer or have gum disease, your dentist may delay the procedure or suggest alternatives. Never get implants without discussing your medication history.
Does MRONJ go away on its own?
Sometimes, but rarely. Early-stage MRONJ (exposed bone with no pain or infection) can stabilize without treatment. But if there’s pain, swelling, or pus, it won’t heal without antibiotics, debridement, or sometimes surgery. Delaying care makes it worse.
Are there alternatives to bisphosphonates that don’t cause jaw problems?
Yes. Romosozumab (Evenity) is a newer drug that builds bone instead of just slowing loss. Teriparatide (Forteo) stimulates new bone growth. Both have lower MRONJ risk than bisphosphonates or denosumab. But they’re more expensive, require injections, and aren’t suitable for everyone. Talk to your doctor about your options.
I’ve been on alendronate for 7 years. Should I stop?
Not unless your doctor recommends it. After five years, your fracture risk drops significantly. Many people benefit from a “drug holiday” after 5-10 years, especially if their bone density has stabilized. But stopping without medical advice increases your fracture risk - and that’s far more dangerous than the tiny chance of MRONJ.
Can I use mouthwash or rinse if I’m on bisphosphonates?
Yes - and you should. Alcohol-free, fluoride-based mouthwashes help reduce bacteria in the mouth, which lowers infection risk. Avoid harsh, acidic rinses. Keep your mouth clean - it’s one of the best defenses against MRONJ.
Next Steps
- If you’re not on bisphosphonates yet: Schedule a dental checkup before starting.
- If you’re currently on them: Book your next dental cleaning. Ask your dentist to check for exposed bone or slow-healing areas.
- If you’ve had a tooth pulled recently and your jaw isn’t healing: See your dentist immediately. Don’t wait.
- If you’re scared to take the medication: Talk to your doctor. Ask: “What’s my personal fracture risk? What’s my personal MRONJ risk?” Numbers help calm fear.








Ajay Brahmandam
21 Dec, 2025
Bisphosphonates saved my grandma’s mobility. She broke her hip at 76, went on alendronate, and walked without a cane for another 8 years. Never had a single dental issue. The fear around MRONJ is way out of proportion to the actual risk. Just get your teeth checked before starting and keep up with cleanings. Simple.
jenny guachamboza
21 Dec, 2025
LOL so you’re telling me Big Pharma doesn’t hide the truth? 🤡 They pump out these drugs knowing they rot your jaw and then tell you it’s ‘rare’ like that makes it okay. I’ve seen 3 people with jaw necrosis - all on Fosamax. Coincidence? I think not. And don’t even get me started on denosumab - that stuff is a chemical time bomb. 🚨💀
Aliyu Sani
22 Dec, 2025
Man, this whole thing hits different when you think about how medicine treats risk as a statistic, not a lived experience. One in a hundred thousand sounds tiny - until it’s your jaw. But then again, not taking the drug? That’s a 50% chance of breaking your hip by 80. It’s not just numbers - it’s your ability to stand up, to walk to the market, to hold your grandchild. The real tragedy isn’t the drug. It’s the system that makes you choose between two kinds of suffering.
Gabriella da Silva Mendes
23 Dec, 2025
Okay but let’s be real - America’s healthcare system is a dumpster fire. Of course people are getting jaw necrosis. We don’t even have universal dental care, and now they want us to take a drug that literally stops bone healing? Meanwhile, Canada and Germany have way lower rates and they don’t even push these meds as hard. This is pure profit-driven medicine. 💸🇺🇸 And don’t even get me started on how dentists don’t even ask about meds until it’s too late. I’m just saying - maybe we should stop treating bones like they’re Lego blocks.
Kiranjit Kaur
24 Dec, 2025
My aunt was terrified of these meds after reading online - she stopped cold turkey and ended up in a wheelchair after a fall. Don’t let fear paralyze you. Talk to your doctor. Get your teeth checked. Stay active. These drugs are tools - not curses. You got this 💪❤️
Sam Black
26 Dec, 2025
I’ve been on Fosamax for 12 years. Had two extractions, a root canal, and a crown - all without a hitch. My dentist says I’m a poster child for ‘low-risk + good hygiene.’ The key isn’t avoiding the drug - it’s avoiding neglect. Brush like your bones depend on it (they do). Floss like your jaw’s a treasure. And don’t let scary stories scare you into inaction. Knowledge > fear.
Cara Hritz
27 Dec, 2025
Wait so you’re saying MRONJ is rare but denosumab is 2x more risky? But then you say both are safer than fractures? So… which one do I pick? I’m confused. Also you spelled ‘bisphosphonates’ wrong in paragraph 3. It’s ‘bisphosphonates’ not ‘bisphosphonates’. Fix that.
Jamison Kissh
28 Dec, 2025
It’s fascinating how we assign moral weight to side effects. We panic over a 0.0007% chance of jaw necrosis but shrug off the 15% lifetime risk of hip fracture. Why? Because one is visible, ugly, and slow - the other is abstract, statistical, and silent. The real question isn’t which drug is safer - it’s why we’re so much more afraid of the visible harm than the invisible one.
Tony Du bled
29 Dec, 2025
My uncle in Australia got on Boniva after a spine fracture. He’s 81 now. Still walks his dog every morning. Never had a dental issue. His dentist says he’s lucky - but I think he’s just smart. He flosses. He doesn’t smoke. He sees his hygienist every six months. The drug didn’t do it. His habits did. Simple as that.
Kathryn Weymouth
29 Dec, 2025
The data presented here is meticulously sourced and accurately contextualized. I appreciate how the post distinguishes between IV and oral bisphosphonates, as well as the nuanced comparison with denosumab. The emphasis on pre-treatment dental evaluation is critical and often overlooked in primary care. This is exactly the kind of evidence-based, patient-centered communication we need more of in public health discourse.
Nader Bsyouni
31 Dec, 2025
So you're telling me the same drug that stops bone turnover to protect your spine also prevents your jaw from healing after a tooth extraction? Sounds like a feature not a bug. Big Pharma knew this all along. They just buried it under a mountain of ‘rare’ and ‘less than lightning’ nonsense. You think your dentist cares? Nah. They get paid per procedure. And you? You’re just a walking wallet with a prescription. Wake up.