When your body mistakes a drug allergy, an immune system overreaction to a medication that can cause symptoms ranging from rash to life-threatening shock. Also known as medication hypersensitivity, it’s not just a side effect—it’s your immune system attacking what it thinks is a threat. Unlike nausea or dizziness, which are common and predictable, a true drug allergy involves your body producing antibodies against the drug, often leading to skin rashes, swelling, trouble breathing, or worse.
Some drugs are more likely to trigger this than others. Penicillin and sulfa antibiotics are top culprits, but even common painkillers like ibuprofen or aspirin can set off reactions in sensitive people. If you’ve ever broken out in hives after taking a new pill, or felt your throat close up after an injection, that’s not just bad luck—it’s a signal your body has flagged that drug as dangerous. And once that happens, the risk stays with you. Re-exposure can make the next reaction even worse.
Many people confuse drug allergies with side effects, but they’re not the same. A side effect is something the drug is known to cause in some people, like drowsiness from antihistamines. A drug allergy is unpredictable and immune-driven. That’s why it’s critical to know the difference. If you think you’re allergic to a medication, don’t just avoid it—you need to document it clearly. Tell every doctor, pharmacist, and nurse. Write it on your phone, your wallet, even your medical alert bracelet. It’s not overkill—it’s lifesaving.
Testing for a drug allergy isn’t always straightforward. Skin tests work well for penicillin, but for most other drugs, doctors rely on your history and careful challenge tests under supervision. If you’ve had a severe reaction, you might never be able to take that drug again. But here’s the good news: sometimes you can. With proper evaluation, many people find they can safely use alternatives or even the same drug under controlled conditions. And for long-term management, allergy shots, a treatment that gradually trains your immune system to tolerate allergens aren’t just for pollen or pet dander—they’re being studied for certain drug allergies too.
If you’ve ever been told you’re allergic to a drug but aren’t sure why, you’re not alone. Studies show up to 90% of people who say they’re allergic to penicillin aren’t actually allergic when tested. That’s a huge problem—it leads to more expensive, less effective, or more dangerous drugs being used instead. Getting the right diagnosis can change your entire treatment path.
And if you’re managing a chronic condition—like autoimmune disease or HIV—you need to know how drug allergies affect your options. Some immunosuppressants or antivirals have cross-reactions. One bad reaction can limit your future care. That’s why knowing your history matters so much. Keep a written list of every drug you’ve reacted to, what happened, and when. Bring it to every appointment.
Below, you’ll find real stories and expert advice on how to spot a drug allergy, what to do if you react, how to talk to your doctor about it, and which alternatives might work when your usual meds are off-limits. Whether you’ve had a mild rash or a scary emergency, this collection gives you the tools to stay safe and get the care you need—without guessing.
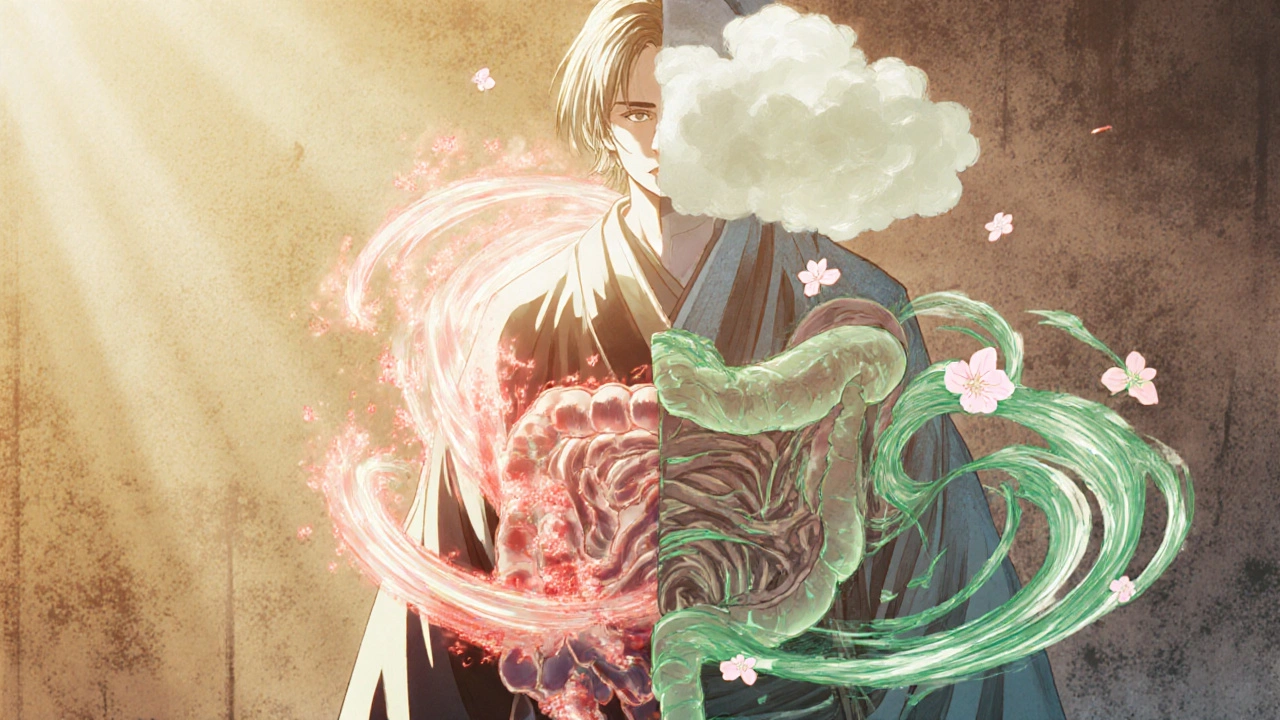
Most drug reactions aren't allergies-they're side effects. Learn how to tell the difference to avoid unnecessary drug avoidance, reduce health risks, and get better treatment options.
CONTINUE READING