When you take a new medication and feel sick, it’s easy to assume you’re allergic. But here’s the truth: most bad reactions aren’t allergies at all. In fact, only 5 to 10% of people who think they have a drug allergy actually do. The rest are experiencing side effects-common, predictable reactions that have nothing to do with your immune system. Mistaking one for the other can cost you more than just discomfort. It can limit your treatment options, raise your risk of infections, and even put your life at risk if you avoid life-saving drugs unnecessarily.
What’s Really Happening in Your Body?
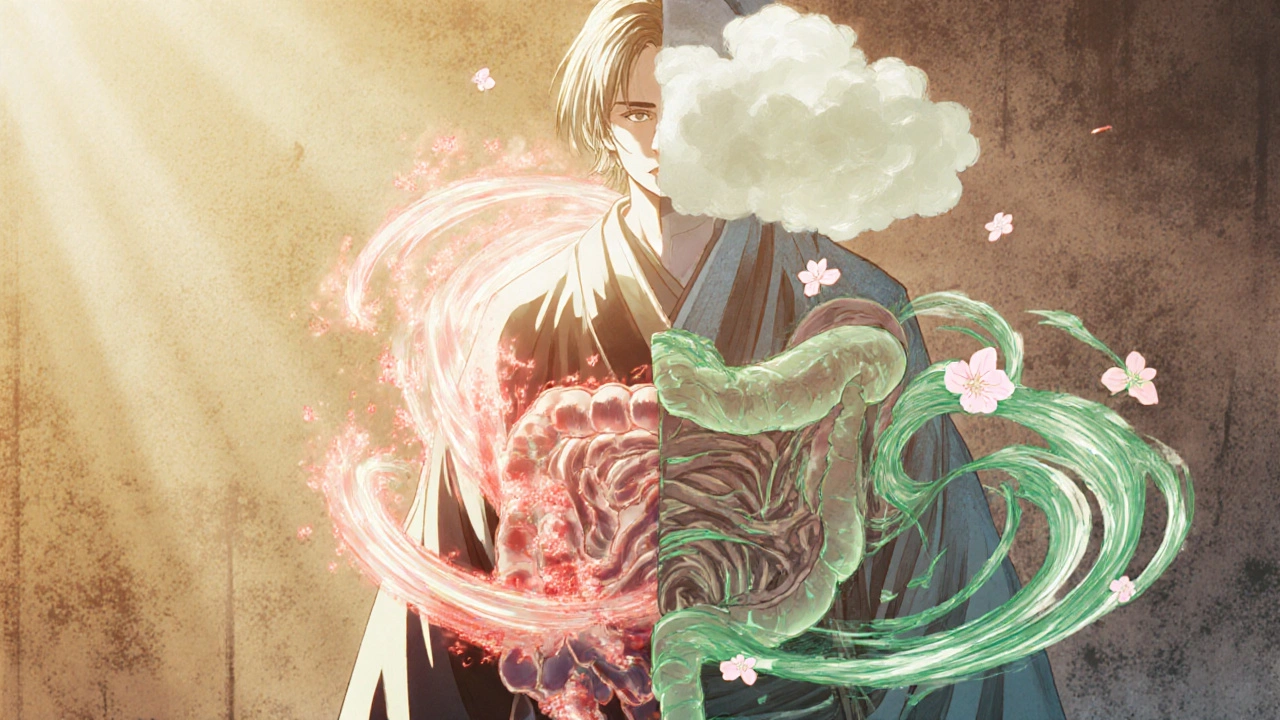
A true drug allergy means your immune system sees the medicine as an invader. It produces antibodies-usually IgE-that trigger a cascade of inflammatory chemicals. That’s what causes hives, swelling, trouble breathing, or anaphylaxis. These reactions don’t just happen because the drug is strong; they happen because your body is fighting it. A side effect is completely different. It’s a direct result of how the drug works in your body. For example, antibiotics like amoxicillin can irritate your gut lining. That’s why nausea and diarrhea are common. It’s not your immune system reacting. It’s the drug doing what it does-just in a place you didn’t expect. Think of it like this: if you eat too much spicy food and get heartburn, that’s a side effect. Your stomach isn’t allergic to chili-it’s just overwhelmed. But if you eat peanuts and your throat closes up, that’s an allergy. Your body is attacking something it thinks is dangerous.Timing Matters: When Did It Happen?
One of the clearest ways to tell the difference is timing. If you got hives, swelling, or trouble breathing within minutes to an hour after taking the drug, that’s a red flag for a true allergy. These are IgE-mediated reactions. They’re fast, they’re intense, and they can get worse with each exposure. Delayed reactions are trickier. A rash that shows up 7 to 14 days after starting a drug could still be an allergy-just not the kind you think of. These are T-cell mediated and often look like a red, flat, itchy rash across your body. Even more serious are reactions like DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms), which can hit 2 to 6 weeks later. DRESS can damage your liver, kidneys, or lungs. It’s rare, but deadly if missed. Side effects? They usually show up fast too-but not because of your immune system. Nausea from antibiotics? It often starts within hours. Dizziness from blood pressure meds? Within a day. The key difference? Side effects usually don’t get worse with repeated doses. They might even fade as your body adjusts.Symptom Patterns: One System or Many?
Side effects usually stick to one system. Nausea? That’s your gut. Headache? That’s your brain. Dizziness? Your inner ear. True allergies? They rarely stay in one place. If you have a rash and swelling and stomach cramps and wheezing-all happening together-that’s a major clue you’re dealing with an immune response. A 2023 analysis of 10,000 patient records found that 87% of true drug allergies involved at least two body systems. Only 22% of side effects did. The most dangerous myth? That nausea means allergy. A 2022 JAMA study found that 68% of people who thought they were allergic to penicillin were actually just nauseous. That’s not an allergy. That’s a side effect. But because they labeled it wrong, they were given stronger, more expensive, and riskier antibiotics instead.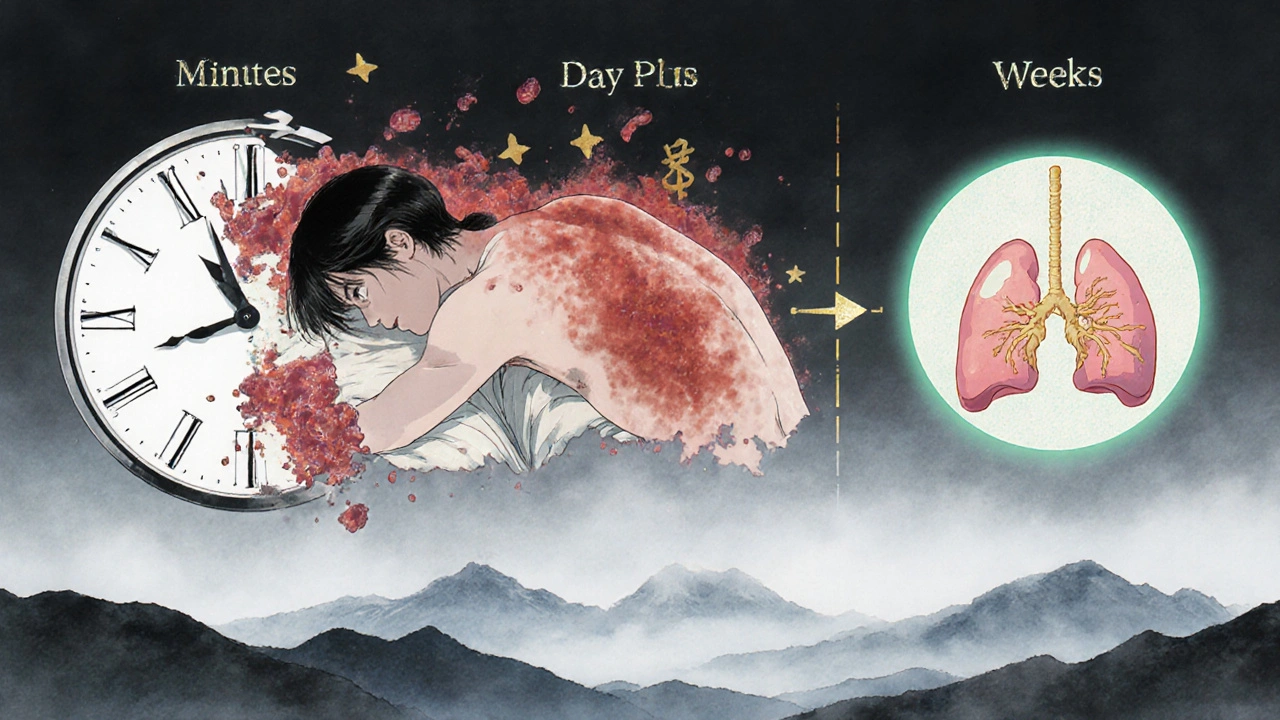
What Happens When You Re-Exposure?
This is one of the most telling signs. If you took the drug again and the same symptoms came back-maybe even worse-that’s a classic sign of an allergy. Your immune system remembers. It’s like a trained guard that now recognizes the intruder. Side effects? They often get better over time. Your body adapts. You might feel queasy the first day of a new painkiller, but by day three, it’s fine. That’s not an allergy. That’s your system adjusting. If you’ve ever stopped a drug because you felt sick, then tried it again and felt fine? You probably didn’t have an allergy. You had a side effect that resolved.What’s the Real Cost of Getting It Wrong?
Mislabeling a side effect as an allergy isn’t just inconvenient-it’s dangerous and expensive. About 7% of Americans say they’re allergic to penicillin. But when tested properly, 90 to 95% of them can take it without issue. That means millions of people are avoiding the safest, cheapest, most effective antibiotic on the planet. Instead, they’re given drugs like vancomycin or clindamycin-drugs that are more likely to cause C. diff infections, kidney damage, or antibiotic resistance. A 2022 JAMA Network Open study showed patients with false penicillin allergies had a 69% higher chance of getting a C. diff infection and stayed in the hospital 30% longer. The CDC estimates incorrect allergy labeling adds $1.1 billion in extra costs to the U.S. healthcare system every year. And it’s not just penicillin. The same problem happens with sulfa drugs, NSAIDs, and even chemotherapy agents. People avoid them because they think they’re allergic-when they’re just intolerant.
What Should You Do If You Think You’re Allergic?
Don’t just assume. Don’t rely on memory from 10 years ago. Don’t let a chart say “penicillin allergy” without asking why. Start with this checklist:- Did the reaction happen within an hour? (If yes, it’s more likely an allergy)
- Did you have hives, swelling, trouble breathing, or dizziness? (These are allergy red flags)
- Did more than one body system react? (Skin + lungs + gut? That’s a strong sign)
- Did symptoms get worse each time you took the drug?
- Did the symptoms go away when you stopped the drug-and come back when you tried it again?






Shannon Amos
27 Nov, 2025
So let me get this straight-I’ve been avoiding penicillin for 12 years because I got a tummy ache once? 🤦♀️ My doctor just nodded and wrote ‘allergy’ like it was a grocery list. Thanks, healthcare system. I’m now on a $500 antibiotic that gives me hiccups and existential dread.
stephen riyo
28 Nov, 2025
I mean... I don't know... I think people just need to stop being so dramatic about side effects? Like, if you're nauseous, maybe you ate too fast? Or drank coffee? Or... I don't know... maybe your body's just being a drama queen? I had a rash once after ibuprofen and I just took a nap and it went away. Not an allergy. Just life.
Wendy Edwards
30 Nov, 2025
OMG YES. I had this exact thing with amoxicillin. Thought I was dying. Rash, fever, felt like I’d been hit by a truck. Went to the ER. They were like ‘nah, DRESS syndrome-rare but real.’ Turned out it WAS an allergy. But then I got tested later and found out I’m fine with penicillin? So now I’m like… wait, did I almost die twice? Or was it just a really bad stomach bug? I’m so confused but also so grateful I didn’t just assume.
Jaspreet Kaur
30 Nov, 2025
The body is a wise thing even when it seems to betray you. We label pain as enemy when often it is just a messenger. A fever does not hate you. Nausea does not condemn you. It speaks in sensations not in diagnoses. To fear a reaction is to fear the language of your own flesh. Learn to listen. Not to panic. Not to erase. To understand.
Gina Banh
2 Dec, 2025
Let’s be real: 90% of ‘drug allergies’ are just people who got sick once and never got tested. I’m a nurse. I’ve seen people avoid beta-blockers because they got dizzy once. Dizziness ≠ allergy. It’s a side effect. You adjust. You take it with food. You don’t get a new label that puts you at risk for C. diff. Stop letting your 2012 experience dictate your 2025 treatment.
Deirdre Wilson
3 Dec, 2025
So like… if I eat a ghost pepper and my mouth catches fire, that’s a side effect? But if I eat a peanut and my throat turns into a deflating balloon, that’s an allergy? Okay. That makes sense. Like… spicy food is just being spicy. Peanuts are like… secret ninja assassins. Got it.
Damon Stangherlin
5 Dec, 2025
This is so important. I used to think I was allergic to sulfa because I got a rash after a UTI med. Turned out it was just dehydration + sun exposure. I got tested last year and now I can take Bactrim again. My doctor said it was the most common mistake he sees. Don’t be the person who avoids the best drug because you thought a headache was your immune system screaming.
Ryan C
5 Dec, 2025
Actually, the 5–10% stat is outdated. A 2024 meta-analysis in JACI showed it’s closer to 3–7% for true IgE-mediated reactions, especially in older adults. Also, DRESS isn’t just ‘rare’-it’s underdiagnosed. And yes, the FDA’s new labeling requirements are a step forward, but EHRs still auto-populate ‘allergy’ from free-text notes. We need AI-driven NLP filters. Also, penicillin skin tests are 98% accurate-not 95%. 📊
Michael Collier
5 Dec, 2025
I appreciate the clarity of this post. As a primary care provider, I see the consequences of mislabeled drug reactions daily. The systemic impact-increased antibiotic resistance, prolonged hospital stays, and unnecessary polypharmacy-is profound. I now routinely refer patients with suspected allergies to our pharmacy-led allergy clinic. Testing is safe, efficient, and often life-changing. Please, if you’ve been labeled allergic, ask for confirmation. You deserve better care.
Dan Rua
6 Dec, 2025
I used to think I was allergic to aspirin because I got a headache after taking it. Turns out I just took it on an empty stomach. Now I always eat first. Also, I got tested last year and they said I’m totally fine. My old chart still says ‘allergy’ though… I had to beg my doctor to fix it. So glad I did. 😊