When you hear bioequivalence, the scientific proof that a generic drug performs the same way in the body as its brand-name version. Also known as drug equivalence, it’s the reason your pharmacy can legally swap your expensive pill for a cheaper one without risking your health. This isn’t marketing fluff—it’s a strict, measurable standard set by the FDA. For a generic to get approved, it must deliver the same amount of active ingredient into your bloodstream at the same speed as the original. No more, no less. If it doesn’t meet that bar, it doesn’t hit shelves.
That’s why generic substitution, when a pharmacist swaps a brand-name drug for a cheaper generic version works without you noticing a difference. It’s not guesswork. Every generic maker runs tests—often with healthy volunteers—to prove their version matches the original down to the milligram and minute. And if you’re on something like warfarin or thyroid meds, where tiny changes matter, the rules are even tighter. The FDA doesn’t just accept claims; they audit the labs, review the data, and sometimes even retest the drugs themselves.
But here’s the thing: not all generics are created equal in people’s minds. Some folks worry that a $5 pill can’t possibly do the same job as a $50 one. But bioequivalence isn’t about price—it’s about science. A study published in the Journal of the American Medical Association tracked over 1,000 patients switching from brand to generic blood pressure meds. No spike in hospital visits. No drop in effectiveness. Just savings—sometimes 80% less. That’s the power of bioequivalence: it lets you keep your health without paying a premium.
Still, confusion lingers. Why? Because bioequivalence doesn’t cover everything. It doesn’t guarantee identical side effects—those can vary due to inactive ingredients like fillers or dyes. And it doesn’t apply to complex drugs like biologics or inhalers, where tiny differences in manufacturing can change how the drug works. That’s why you’ll see posts here about FDA approval, the official process that verifies a drug’s safety, effectiveness, and bioequivalence before it reaches patients, and why some people need to fight insurance to keep their brand-name drug. But for most common meds—antibiotics, statins, antidepressants—bioequivalence is your quiet ally. It’s the invisible rule that keeps generics safe, legal, and affordable.
Below, you’ll find real stories and guides about how this plays out in practice: when insurance forces a switch, when buying abroad gets tricky, how pharmacists help you navigate it all, and what to do if you think your generic isn’t working right. These aren’t theoretical debates. They’re everyday decisions—made easier when you understand what bioequivalence really means.
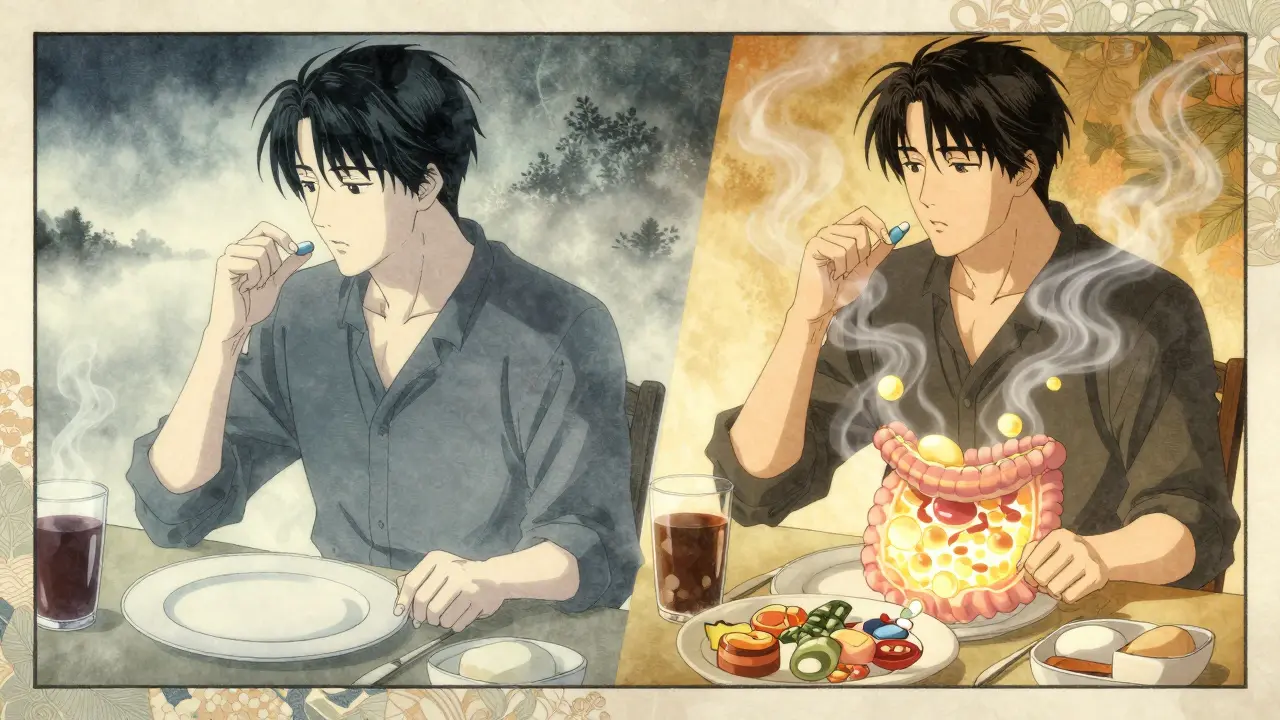
Fasted and fed state testing reveal how food impacts drug absorption and exercise performance. Understanding both conditions ensures accurate dosing, effective training, and better health outcomes.
CONTINUE READING