What Exactly Are Sleepwalking and Night Terrors?
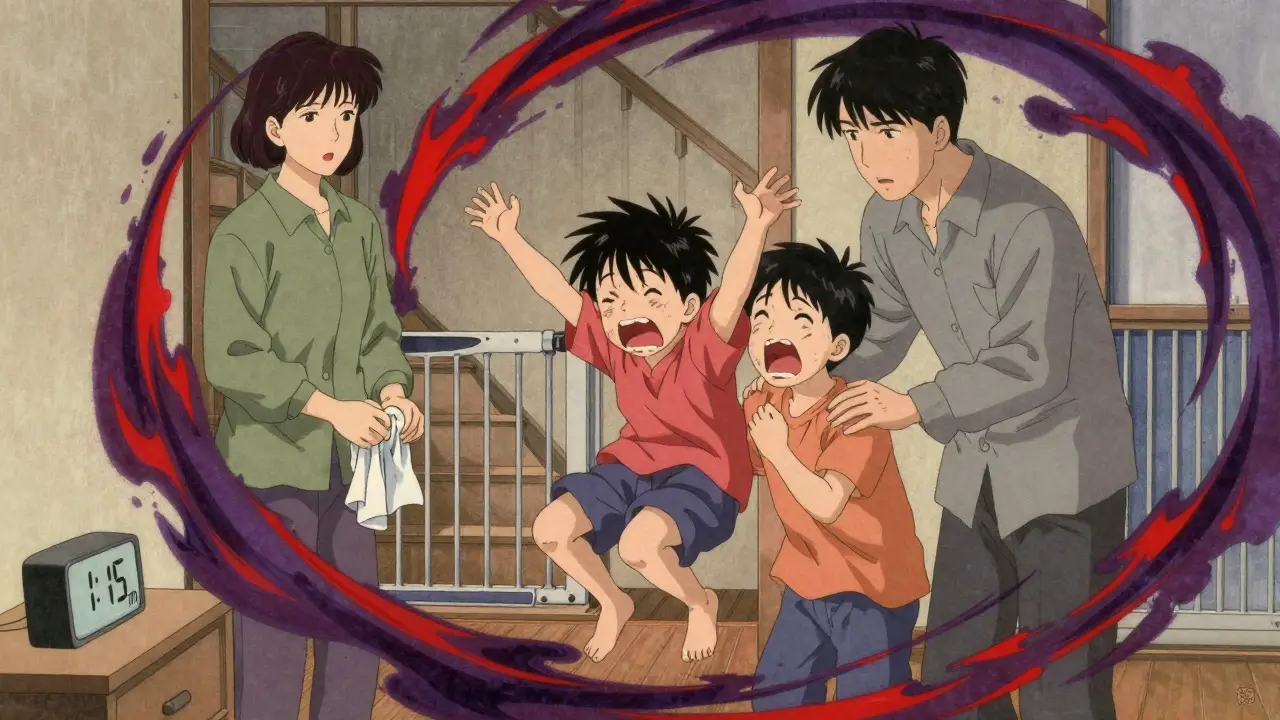
Think of sleepwalking and night terrors as your brain getting stuck halfway between deep sleep and waking up. These aren’t dreams you remember. They’re not nightmares. They’re parasomnias - physical events that happen during deep NREM sleep, usually within the first two hours after falling asleep. You might sit up screaming, bolt out of bed, or even walk downstairs and start making toast. Then, you go right back to sleep. In the morning, you remember nothing.
It’s more common in kids. About 1 in 5 children sleepwalk at least once, and 1 in 10 have night terrors. Most grow out of it by their teens. But adults can have them too - about 1 in 25. And when they do, it’s often a sign something else is going on, like sleep apnea, stress, or an underlying neurological issue.
Why Do These Episodes Happen?
It’s not about stress alone. It’s about deep sleep pressure. When your brain is overloaded with slow-wave sleep - the kind that happens early in the night - it can glitch. The part of your brain that controls movement doesn’t fully shut down, even though your conscious mind is still asleep.
For night terrors, your body goes into full panic mode: heart rate spikes to 120-140 beats per minute, you sweat heavily, and your breathing gets fast and shallow. You’re not scared of a monster - your nervous system is just firing on all cylinders. For sleepwalking, your motor system is active. You might open doors, turn on lights, or even drive a car. You’re not dreaming it. You’re doing it.
And here’s the kicker: 95% of people have zero memory of it. That’s why families are often the first to notice. A child screaming in the middle of the night isn’t being dramatic. They’re trapped in a neurological glitch.
How to Keep Someone Safe During an Episode
Safety is the first and most important step. No medication, no therapy - nothing matters if someone gets hurt.
- Lock all doors and windows. Use alarms that beep when a door opens. These cost less than $30 and are used by 92% of sleep specialists.
- Remove sharp objects from the bedroom. Knives, glass, tools - anything within 10 feet of the bed.
- Put the mattress on the floor. Falls are the #1 cause of injury. This cuts fall-related injuries by 75%.
- Don’t try to wake someone during a night terror. You’ll likely make it worse. Instead, gently guide them back to bed. Speak calmly. Don’t grab or shake them.
- If they sleepwalk, clear the path. Block stairs with baby gates. Install motion-sensor night lights so they don’t trip in the dark.
One parent in Adelaide told me her 6-year-old used to walk to the kitchen and open the fridge every night. She installed a door alarm. Within two weeks, the episodes dropped by 80%. No meds. Just safety.
Scheduled Awakenings: A Proven Trick for Sleepwalking
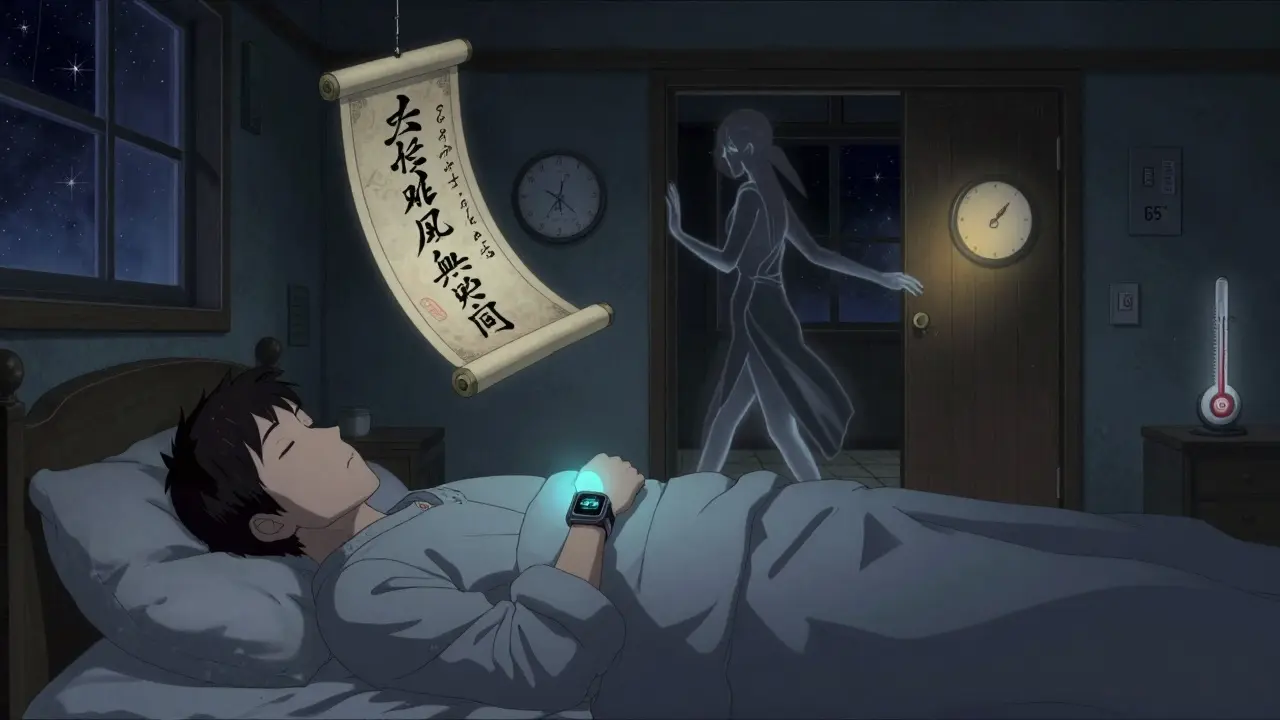
If sleepwalking happens at the same time every night - say, 1:15 a.m. - you can interrupt it before it starts.
Here’s how:
- Figure out the typical time of the episode. Keep a sleep diary for two weeks.
- Set an alarm to wake the person 15 to 30 minutes before that time.
- Keep them fully awake for 5 minutes. Talk to them, give them water, let them sit up.
- Let them go back to sleep.
- Do this every night for 7 to 14 days.
This works because you’re disrupting the deep sleep cycle before the brain glitches. Studies show 70-80% of kids and adults see a major drop in episodes. It’s not magic. It’s timing.
What About Night Terrors? Can They Be Treated?
Night terrors don’t respond to scheduled awakenings as well as sleepwalking. But they do respond to sleep extension.
Most kids and adults with night terrors are chronically sleep-deprived. They’re not getting enough total sleep. That pushes their brain deeper into slow-wave sleep - the exact state where terrors happen.
Try adding 30 to 60 minutes to their bedtime. If they normally sleep 8 hours, aim for 8.5 to 9. Do this for 4 weeks. In clinical studies, this alone reduces episodes by 65%.
Also, keep the room cool - between 60 and 67°F. Heat increases slow-wave sleep pressure. A cooler room = less deep sleep = fewer terrors.
When to See a Doctor
Most kids outgrow this. But adults? That’s different.
See a sleep specialist if:
- Episodes happen more than twice a week.
- There’s violence - hitting, kicking, yelling aggressively.
- The person is confused for more than 15 minutes after waking.
- It started in adulthood. Adult-onset parasomnias can signal sleep apnea, Parkinson’s, or seizures.
- They’re injuring themselves or others.
Doctors use polysomnography - an overnight sleep study with video and brainwave monitoring - to confirm it’s not epilepsy or REM sleep behavior disorder. About 30-40% of adult cases are linked to another sleep disorder. Treating that often fixes the parasomnia.
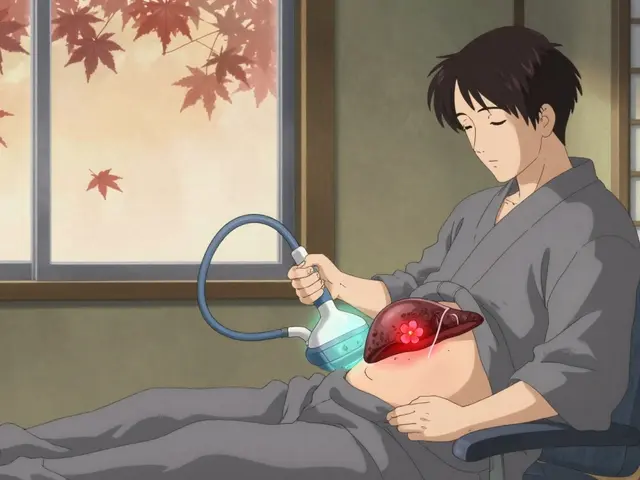
Medications: Only When Necessary
Medication is a last resort. Most doctors won’t touch it unless episodes are frequent and dangerous.
Clonazepam (a benzodiazepine) helps about 60-70% of people. But it can cause drowsiness, dependence, and memory issues. It’s not for long-term use.
Melatonin is safer. It helps regulate sleep cycles and reduces episodes in 40-50% of cases. Dose: 3-6 mg taken 30 minutes before bed.
There’s a new FDA-approved option: Nightware. It’s an Apple Watch app that detects rising heart rate before a night terror hits - then gently vibrates to nudge the brain back to normal sleep. In trials, it cut episodes by 35% over six months. No pills. No side effects.
What Doesn’t Work
Don’t rely on these:
- “Just wake them up.” That makes night terrors worse.
- “They’re just acting out.” It’s not behavioral. It’s neurological.
- “They’ll grow out of it.” True for kids, but not for adults. Adult cases don’t resolve on their own.
- “Sleeping pills will help.” They often make it worse by deepening slow-wave sleep.
Long-Term Outlook
For kids: 80-90% stop by age 12. No treatment needed - just safety and patience.
For adults: With the right combo of sleep extension, safety, and therapy, 60-70% see major improvement. Cognitive behavioral therapy for parasomnias (CBT-P) is now available in digital form - apps like Sleepio deliver structured sessions over 8 weeks and cut sleepwalking by nearly half.
Genetics play a role too. If someone in your family sleepwalks, you’re more likely to. A 2023 study found a gene variant (DEC2) linked to familial sleepwalking with 87% accuracy.
Final Takeaway
Sleepwalking and night terrors aren’t scary because they’re supernatural. They’re scary because they’re unpredictable. But they’re manageable. You don’t need to live in fear. Start with safety. Add consistent sleep. Try scheduled awakenings or sleep extension. If it’s still happening after a few months, see a sleep specialist. Most cases respond well - without pills, without panic, without shame.
Are sleepwalking and night terrors the same thing?
No. Sleepwalking involves physical movement - walking, opening doors, even driving. Night terrors involve intense fear, screaming, and autonomic arousal (fast heart rate, sweating), but no purposeful movement. Both happen during deep NREM sleep, but night terrors are more about panic, while sleepwalking is about action. Neither involves dream recall.
Can adults have sleepwalking or night terrors?
Yes. While they’re more common in children, 1-4% of adults experience them. Adult-onset cases are often linked to other conditions like sleep apnea, stress, PTSD, or neurological disorders. If it starts after age 18, it’s not normal childhood behavior - it needs medical evaluation.
Should I wake someone during a night terror?
No. Trying to wake someone during a night terror can make them more agitated or confused. Instead, stay calm, speak softly, and gently guide them back to bed. Most episodes last under 5 minutes. They’ll settle down on their own.
Is it dangerous to sleepwalk?
Yes, especially if safety isn’t addressed. People have fallen down stairs, walked into traffic, or handled knives while sleepwalking. Minor injuries like cuts and bruises are common. Severe injuries like fractures or head trauma happen in about 8% of cases. Prevention through environmental safety is critical.
Can sleepwalking be cured?
In children, yes - most outgrow it. In adults, it can be controlled. Scheduled awakenings, sleep extension, and CBT-P reduce episodes by 70% or more. Medication can help in severe cases, but it’s not a cure. The goal is management, not elimination.
Do I need a sleep study to diagnose this?
Not always. For children with typical symptoms and no injury risk, a detailed history is often enough. But for adults, frequent episodes, violence, or new-onset symptoms, a sleep study (polysomnography) is recommended to rule out seizures, sleep apnea, or REM sleep behavior disorder.








Maggie Noe
10 Jan, 2026
I used to sleepwalk as a kid and my mom would just leave a trail of snacks from my room to the kitchen 😅 One time I made a PB&J and went back to bed. No memory of it. My parents still laugh about it. Now I’m 32 and it stopped cold. Guess my brain just grew up.
Darren McGuff
10 Jan, 2026
As a sleep specialist for 18 years, I’ve seen this a thousand times. Scheduled awakenings? Absolute gold. Works better than meds for 70% of kids. And for adults? Sleep extension is the quiet hero. Most people think it’s ‘stress’-nah. It’s sleep debt. Fix the foundation, and the house stops collapsing. No pills needed.
Ashley Kronenwetter
11 Jan, 2026
While the information presented is largely accurate, I must emphasize the importance of consulting a board-certified sleep physician before implementing any intervention, particularly in adult populations. The differential diagnosis for parasomnias is complex and requires clinical evaluation to exclude seizure disorders, REM sleep behavior disorder, and other neurological conditions.
Heather Wilson
12 Jan, 2026
I’m sorry, but this article feels dangerously oversimplified. You say ‘don’t wake them’ like it’s gospel, but what if they’re about to walk into traffic? What if they’re holding a knife? You talk about safety like it’s optional. And then you casually mention melatonin like it’s candy. Did you even read the FDA warnings? People die from this. This isn’t a parenting blog-it’s a medical emergency waiting to happen.
Jeffrey Hu
13 Jan, 2026
You missed the real culprit: blue light. Everyone’s on their phones till midnight. That kills melatonin production. No wonder people are sleepwalking. It’s not the sleep cycle-it’s the screen addiction. And don’t get me started on Nightware. Apple Watch vibrates? That’s not science, that’s marketing. Real treatment is CBT-I, not fancy gadgets. Also, 6mg melatonin? That’s a drug dose. 0.3mg is the real number. You’re giving people poison.
Matthew Maxwell
14 Jan, 2026
This is what happens when we stop respecting natural order. Back in my day, kids went to bed at 8, didn’t have phones, and didn’t sleepwalk because their parents had discipline. Now we treat sleepwalking like it’s a cute quirk. It’s not. It’s a sign of moral decay in parenting. You let your kid wander the house at 2 a.m.? You’re not a parent-you’re a bystander. Wake them. Scare them straight. That’s what discipline looks like.
Kiruthiga Udayakumar
16 Jan, 2026
My cousin in India had night terrors since she was 5. Her grandma used to whisper mantras in her ear and sprinkle turmeric water around the bed. No doctor. No alarms. Just faith. And guess what? After 3 years, it vanished. Science is great, but sometimes the old ways work better. Maybe we’re overcomplicating this. The soul knows what the brain forgets.
Patty Walters
17 Jan, 2026
I’ve been sleepwalking since I was 7. Now I’m 41. I’ve fallen down stairs, opened the fridge in my underwear, and once tried to ‘drive’ my bike in the living room. I use motion lights, mattress on floor, door alarms. And I go to bed at the same time every night-no exceptions. It’s not perfect, but I haven’t had an episode in 11 months. Small changes, big difference. Also, sleepio app? Life saver. I’m not even kidding.
Jenci Spradlin
18 Jan, 2026
I’m a nurse and I’ve seen this up close. One time a guy sleepwalked into the ER because he thought he was at work. He was trying to ‘check vitals’ on the receptionist. No meds, no trauma-just pure sleep glitch. The trick? Keep the room cool. Like, 65°F. Heat makes your brain go deeper into that glitch zone. And yeah, scheduled awakenings work. I’ve done it with my own kid. 2 weeks, no more walking. Simple. No drama.
Gregory Clayton
19 Jan, 2026
Y’all are overthinking this. My cousin in Texas sleepwalked for 12 years. One night he drove his pickup to the gas station, bought a Slurpee, and went back to bed. The next day he asked why his shirt was sticky. That’s it. No alarms. No apps. No therapy. He just stopped one day. Maybe your brain just gets tired of the drama. Let it rest. Or move to Alaska. Cold helps. I swear.