When you pick up a prescription at the pharmacy, you might not think about why your copay for a generic pill is $5 while the brand-name version costs $50. That difference isn’t random-it’s the result of a carefully engineered system called insurance benefit design. Health plans and pharmacy benefit managers (PBMs) use this system to control rising drug costs, and generics are their most powerful tool.
Why Generics Are the Backbone of Cost Control
Generic drugs are chemically identical to their brand-name counterparts but cost 80-85% less. In 2022, 91.5% of all prescriptions filled in the U.S. were for generics, yet they made up only 22% of total drug spending. That’s the math behind the savings: 9 out of 10 prescriptions are cheap, but they only add up to a fraction of the bill. Over the past decade, generics saved the U.S. healthcare system more than $3.7 trillion. In 2022 alone, that number was over $370 billion. This isn’t just about big numbers. For a patient taking a monthly blood pressure pill, switching from brand-name Lisinopril to its generic version can cut their monthly cost from $45 to $4. That’s $500 saved per year. For someone on multiple medications, the savings can be thousands.How Plans Push Patients Toward Generics
Insurance plans don’t just hope people choose generics-they design systems to make it the easiest, cheapest, and sometimes only option. Tiered formularies are the most common tool. Most plans divide drugs into tiers, with generics in Tier 1. Copays for Tier 1 generics are often $0-$10 for a 30-day supply. Preferred brand drugs sit in Tier 2 with copays of $25-$50. Non-preferred brands? That’s Tier 3, where you might pay $60-$100 or more. The gap isn’t accidental-it’s intentional. The bigger the difference, the stronger the incentive to pick the generic. Mandatory substitution is another lever. All 50 states allow pharmacists to swap a brand-name drug for its generic equivalent unless the doctor specifically says “dispense as written.” That means even if your doctor prescribes a brand, the pharmacist can legally give you the generic unless blocked. Step therapy requires you to try the generic first. If it doesn’t work, then you can appeal for the brand. As of 2023, 92% of Medicare Part D plans use step therapy. That means if you’re on a brand-name statin, your plan will make you try atorvastatin (generic Lipitor) before approving the more expensive alternative. Closed formularies go even further. Some plans, especially in Medicare Advantage and Medicaid, don’t cover the brand-name drug at all if a generic exists. One Medicare HMO study found that switching to a closed formulary reduced brand-name use by nearly 30%-without increasing hospital visits or complications.Who’s Really Saving Money?
On paper, everyone wins: insurers pay less, employers save on premiums, and patients pay lower copays. But the reality is more complicated. The big middlemen-PBMs like CVS Caremark, OptumRx, and Express Scripts-negotiate prices between drugmakers and pharmacies. They claim they pass savings to plans. But research from the USC Schaeffer Center shows patients often pay more than they should. How? Through spread pricing and copay clawbacks. Spread pricing means the PBM tells the insurer, “This generic costs $15,” but only pays the pharmacy $8. The $7 difference goes to the PBM. The patient pays their $10 copay, thinking they’re getting a deal. But the PBM pockets the difference. In some cases, patients end up paying more than the actual cost of the drug. Copay clawbacks happen when your copay is based on the brand-name price, but you get the generic. The plan collects your copay, then refunds the difference to the pharmacy-but not to you. So you pay $25 for a $5 drug, and the plan keeps the $20. You’re not saving-you’re being overcharged. A 2024 Department of Labor report found that 14% of patients paid $10-$15 more than they should have for generics due to these practices.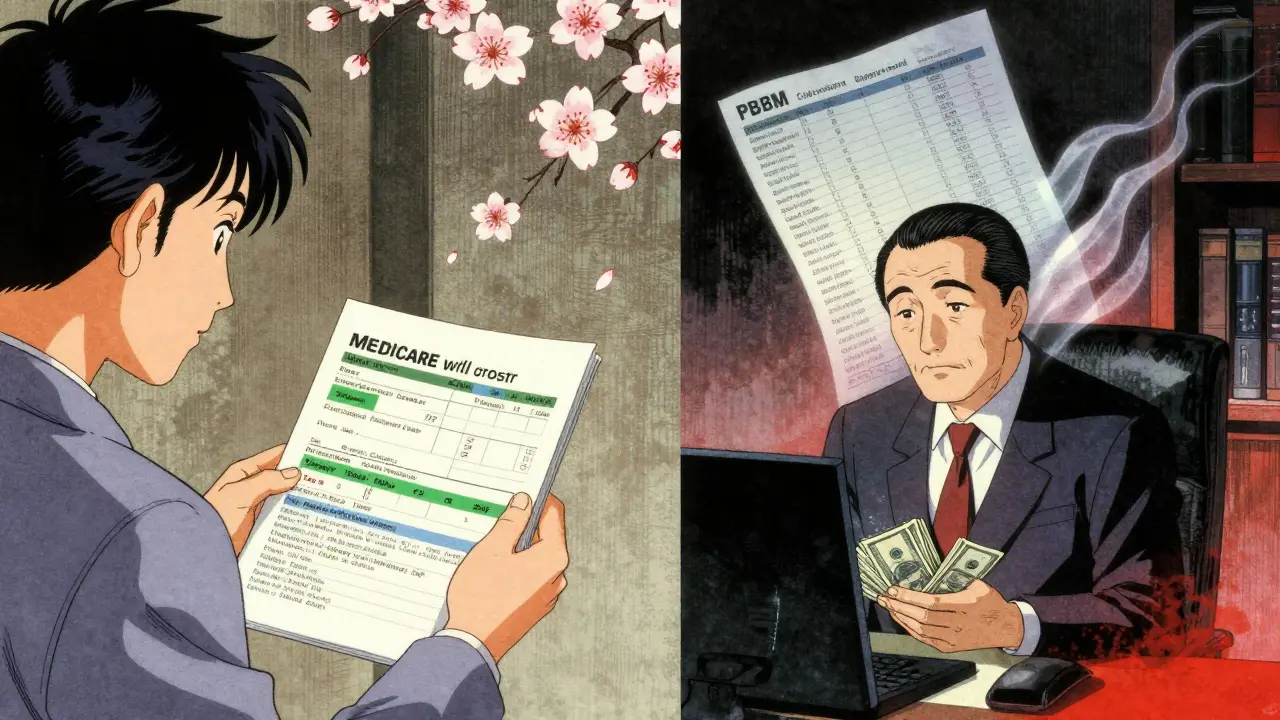
How Different Plans Compare
Not all insurance plans treat generics the same way. Medicare Part D plans cover 50 million seniors. They all use tiered formularies, and most have $0-$15 copays for generics. But out-of-pocket caps changed in 2025: now, no senior pays more than $2,000 a year for drugs. That’s forced plans to rethink how they use generics-not just to save money, but to help patients hit the cap faster. Medicaid has federal rules that cap what states can pay for generics at 250% of the average manufacturer price. In 2022, Medicaid had a generic dispensing rate of 89.3%, slightly higher than commercial plans. States are now testing new models like the GENEROUS Model, launching in 2026, which will let CMS negotiate directly with generic makers to drive prices even lower. Commercial plans are shifting toward high-deductible health plans (HDHPs) with Health Savings Accounts (HSAs). Even before the deductible is met, many of these plans offer $0 copays for generics. That’s because the goal isn’t just to reduce claims-it’s to encourage smart spending early on. Self-insured employers are often the most aggressive. A 2021 Johns Hopkins study found two large employers saved 9-15% on drug costs by switching to lower-cost alternatives-without any drop in health outcomes. They didn’t just rely on PBMs; they built their own drug substitution programs.What Patients Really Experience
Real people don’t always see the savings they’re promised. On Reddit, a thread titled “Generic drug copay went from $5 to $0 last month-anyone else?” got 142 comments. Eighty-seven percent said it was a game-changer. But 13% said they couldn’t get certain generics because their plan didn’t cover them. One woman reported being switched from a brand-name thyroid med to a generic, then having to go back to the brand because her symptoms returned. Her doctor had to file three appeals. A Kaiser Family Foundation survey found that while 68% of Medicare beneficiaries were satisfied with their generic coverage, 22% had trouble getting prior authorization for brand-name drugs-even when their doctor said the generic wasn’t working. Fourteen percent said their doctor had to appeal multiple times. And then there’s the confusion. Only 38% of Medicare beneficiaries understood how their plan’s generic coverage worked in 2023. They didn’t know about tiers, copay differences, or step therapy. That’s not their fault-it’s a system designed by actuaries, not patients.
The Future of Generic Benefit Design
Change is coming. The Inflation Reduction Act gives Medicare the power to negotiate drug prices, starting in 2026. That will affect both brand-name and generic drugs. The first set of negotiated prices will roll out for Part D drugs in 2026, and for Part B in 2028. The GENEROUS Model for Medicaid, launching in 2026, could save $40 billion over ten years by standardizing coverage rules and negotiating directly with manufacturers. It’s a direct challenge to the current PBM model. New players are entering the game, too. The Mark Cuban Cost Plus Drug Company sells 124 generics at transparent, cost-plus prices-no PBM, no spread, no clawback. In 2023, patients saved a median of $4.96 per prescription. But here’s the catch: Medicaid patients saw no savings. That’s because Medicaid already pays low prices. The real winners are the uninsured and those on high-deductible plans. Starting January 1, 2025, insurers must show detailed breakdowns of drug costs on Explanation of Benefits (EOB) statements. That means you’ll finally see what the PBM paid, what the pharmacy paid, and what you paid. No more hiding.What You Can Do
You don’t have to be a policy expert to benefit from this system. Here’s how to make it work for you:- Always ask your pharmacist: “Is there a generic version?” Even if your doctor didn’t prescribe one, it might be available.
- Check your plan’s formulary online. Look for tier numbers and copays. Know where your meds sit.
- If your copay for a generic is higher than expected, call your insurer. Ask: “Is this a spread pricing situation?”
- If a generic isn’t working, ask your doctor to write “dispense as written.” You have the right to appeal if your plan denies it.
- Compare prices. Sometimes buying a generic directly from a cash pharmacy like Walmart or Costco is cheaper than using your insurance.
Final Thoughts
Generic drugs aren’t a magic fix. They’re a tool-and like any tool, they can be used well or poorly. Insurance plans use them to save money. PBMs use them to make profits. Patients use them to stay healthy. The system works best when transparency replaces complexity. When patients understand their copays, when savings actually reach them, and when doctors and pharmacists can choose what’s best-not what’s cheapest for the middleman. The next time you pick up a prescription, remember: that little pill might be saving you hundreds. But only if the system is working the way it should.Why is my generic drug copay higher than expected?
Your copay might be higher because your insurance plan or pharmacy benefit manager (PBM) uses spread pricing. This means they charge your plan one price for the generic, pay the pharmacy less, and keep the difference. You pay your copay based on the inflated price, not the actual cost. Some plans also have copay clawbacks, where you pay a brand-name copay even when you get the generic, and the plan keeps the difference. Check your Explanation of Benefits (EOB) statement-starting in 2025, it must show exactly what was paid.
Can I refuse a generic drug if my plan forces me to take it?
Yes. If your plan requires you to try a generic first (step therapy) or automatically substitutes it, you can ask your doctor to write “dispense as written” on the prescription. You also have the right to appeal if the generic doesn’t work for you or causes side effects. Many plans require multiple appeals, so document your symptoms and keep copies of all correspondence.
Do all insurance plans cover generics the same way?
No. Medicare Part D plans must use tiered formularies but vary in copay amounts. Medicaid plans have state-specific rules and often have higher generic dispensing rates. Commercial plans differ widely-some offer $0 generics even before you meet your deductible, while others have higher copays. Self-insured employers often have the most aggressive generic programs because they pay claims directly, not through a PBM.
Are generic drugs really as effective as brand-name ones?
Yes. The FDA requires generics to be bioequivalent to brand-name drugs-meaning they work the same way in the body. Studies show no difference in effectiveness for most medications. However, a small percentage of patients report side effects or reduced effectiveness after switching, especially with drugs that have narrow therapeutic windows (like thyroid meds or seizure drugs). If you notice a change after switching, talk to your doctor.
How do I know if my plan is using a closed formulary?
Check your plan’s formulary document, usually available online. If a brand-name drug isn’t listed at all, even under a higher tier, it’s likely excluded because a generic exists. Closed formularies are common in Medicare Advantage and Medicaid plans. If you’re prescribed a brand-name drug that’s not covered, your doctor may need to file a prior authorization or exception request.
Will the new Medicare drug price negotiation affect generics?
The Inflation Reduction Act’s price negotiation rules apply to both brand-name and generic drugs, but only to those with no generic competition. Once a generic is available, Medicare can’t negotiate the brand-name price. So while negotiation won’t directly lower generic prices, it could reduce the demand for brand-name drugs, indirectly strengthening the position of generics in formularies.











bhushan telavane
21 Dec, 2025
India's generic drug scene is wild-cheap as hell, but sometimes the quality feels like a lottery. I’ve had my blood pressure med switch twice in a year, and each time my head spins for a week. No one tells you that generics aren’t all created equal, even if the FDA says they are.
Nancy Kou
22 Dec, 2025
My dad’s on 7 meds. Switched to generics last year-his monthly bill dropped from $320 to $47. We cried. Not because we were sad, but because we finally had breathing room. This system works when it’s not rigged by middlemen.
Hussien SLeiman
23 Dec, 2025
Let’s be real-this whole ‘generics save money’ narrative is corporate propaganda wrapped in a lab coat. PBMs are the real villains, not the drug companies. You think the $5 generic is a gift? Nah. It’s a trap. They lower the price just enough to make you feel smart for choosing it, then they jack up the copay based on the brand’s inflated list price. And don’t get me started on ‘step therapy’-it’s not medical protocol, it’s financial coercion disguised as care. The system doesn’t care if you’re stable, only if you’re cheap.
And now Medicare’s going to ‘negotiate’ prices? Like that’ll change anything. The same players who ran the game before are still running it. The only thing that’s changed is the branding. You think a $40 billion Medicaid savings model is about patient care? It’s about shifting the burden from insurers to taxpayers. Wake up.
And yes, I’ve read the studies. I’ve seen the data. But data doesn’t tell you about the 82-year-old woman who had to wait six weeks for an appeal to get her brand-name thyroid med back because the generic made her heart race. Her doctor’s notes? Ignored. Her pain? A line item.
Generics aren’t the problem. The profit-driven architecture around them is. And until we remove PBMs from the equation entirely, we’re just rearranging deck chairs on the Titanic.
Aadil Munshi
24 Dec, 2025
Classic case of ‘the math looks good until you realize the math was written by someone who’s never held a pill bottle.’ Generics are 80% cheaper? Sure. But if your copay is based on the brand’s list price, you’re paying more than the actual cost of the drug. That’s not savings-that’s theft with a pharmacy receipt.
And don’t even get me started on ‘dispense as written.’ Good luck getting a doctor to fight for you. Most are overworked, underpaid, and scared of PBM retaliation. So they just write the generic and hope for the best. Meanwhile, you’re stuck with a pill that makes you dizzy because the filler’s different.
Also, Mark Cuban’s drug company? Cute. But it only works for people who can pay cash. What about the 40% of Americans who can’t afford $20 out of pocket, even for a $5 generic? The system doesn’t fix itself-it just creates new loopholes for the rich to exploit.
And yes, I know the FDA says generics are bioequivalent. But bioequivalent doesn’t mean ‘same experience.’ I’ve been on the same SSRI for 12 years. Switched to generic. Got migraines for three weeks. Went back to brand. Felt like a new person. My doctor said ‘it’s all in your head.’ It wasn’t.
Frank Drewery
25 Dec, 2025
I just want to say thank you for writing this. My mom’s on dialysis and takes 11 meds. She used to skip doses because she couldn’t afford them. Now, thanks to generics and a good Medicare plan, she’s stable. It’s not perfect, but it’s better than before. Keep pushing for transparency.
Danielle Stewart
27 Dec, 2025
As a pharmacist, I see this every day. Patients think generics are ‘inferior’ because they’re cheaper. They’re not. But the system makes them feel guilty for wanting the brand. I’ve had people cry because their insurance won’t cover their brand-name seizure med-even though the generic caused them to have a seizure. We’re not just talking about money here. We’re talking about lives.
Always check your EOB. Always ask for the generic cost vs. your copay. And if your plan says ‘you paid $25 for a $5 drug,’ call them. They’ll usually fix it. Most of the time, it’s a system error. But sometimes? It’s intentional. Don’t let them gaslight you.
jessica .
28 Dec, 2025
THEY’RE NOT EVEN THE SAME DRUG. THE GOVERNMENT LETS THEM CHANGE THE FILLERS AND THE COLOR AND THE SHAPE AND THEN TELLS US IT’S THE SAME?!? THIS IS A BIG PHARMA CONSPIRACY TO CONTROL US. THEY’RE PUTTING LYE IN THE GENERIC VERSIONS TO MAKE US DEPENDENT ON THE BRANDS. I SAW IT ON A YOUTUBE VIDEO. THE FDA IS IN THE POCKET OF THE PBMS. TRUMP KNEW THIS. BIDEN IS A PUPPET. THEY WANT YOU TO BE SICK SO THEY CAN SELL YOU MORE DRUGS. CHECK YOUR EOB. THEY’RE HIDING THE TRUTH.
Ryan van Leent
28 Dec, 2025
Why do people even care about this? Just pay the $5. If you can’t afford $5 a month for your meds, maybe you shouldn’t be taking them. I mean, I get it, you’re poor, but this is why we have food stamps and Medicaid. Stop whining about the system and fix your life. Also, why are you even on Reddit reading this? Go get a job.
Sajith Shams
29 Dec, 2025
Let me break this down for the people who think generics are ‘the solution.’ The U.S. doesn’t regulate generic manufacturers the same way it does brand-name ones. Many generics are made in India and China. The FDA inspects less than 2% of those factories. So when your generic ‘doesn’t work,’ it’s not placebo-it’s because the active ingredient is 7% under the required threshold. And guess who gets sued when you have a stroke? Not the PBM. Not the pharmacy. The patient. You’re the liability.
And step therapy? It’s not ‘try the cheap one first.’ It’s ‘delay care until you’re in crisis.’ That’s not healthcare. That’s actuarial risk management. And the fact that 92% of Medicare plans use it? That’s not innovation. That’s negligence.
Also, the ‘GENEROUS Model’? Sounds like a PR stunt. The same companies that run PBMs are lobbying for it. They’ll just rename the scam. You think they want lower prices? They want more control. More leverage. More profit. Always.
Adrienne Dagg
30 Dec, 2025
OMG I JUST REALIZED MY COPAY FOR GENERIC LISINOPRIL IS $15 BUT THE ACTUAL COST IS $3?? I’M SO MAD 😤 I’M CALLING MY INSURANCE TOMORROW AND I’M TELLING THEM TO FIX IT. THIS IS INSANE. 🤬 #GenericScam #SpreadPricingIsTheft