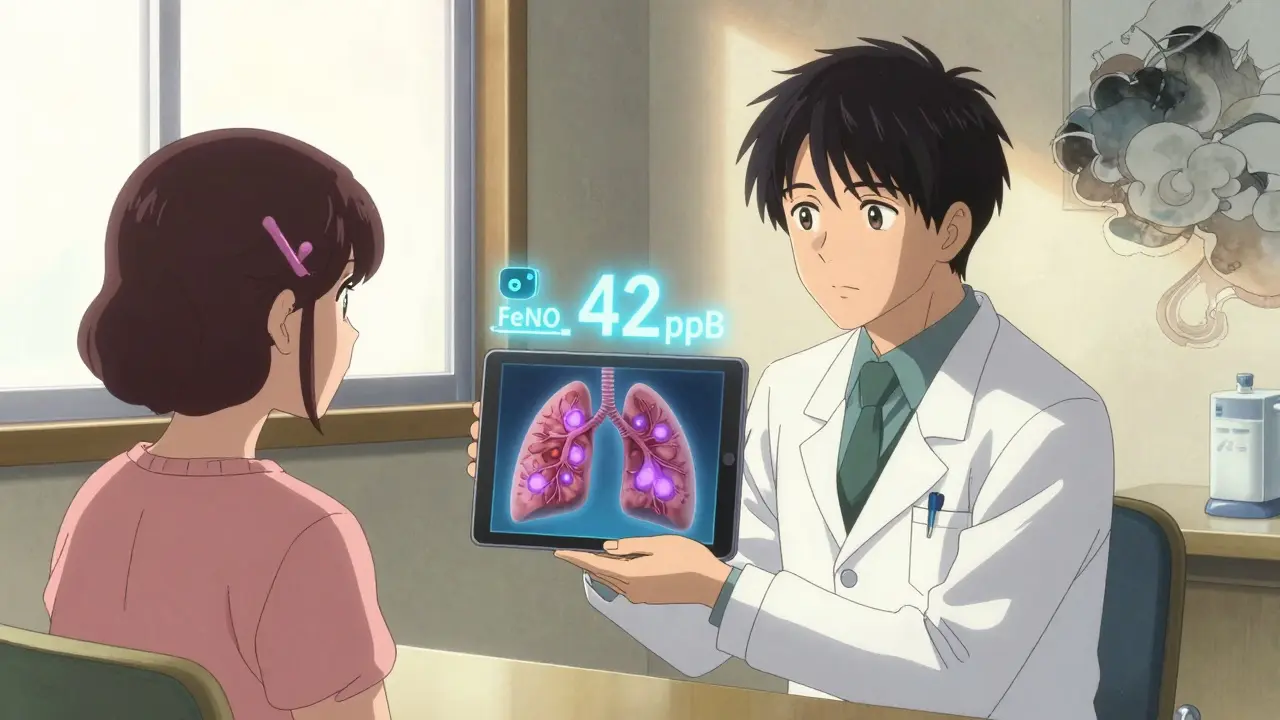
When your asthma isn’t under control, it’s easy to blame yourself. Maybe you didn’t take your inhaler enough. Maybe you missed a trigger. But what if the problem isn’t you - it’s that your doctor can’t see what’s happening inside your airways? That’s where FeNO testing changes everything.
What FeNO Testing Actually Measures
FeNO stands for Fractional Exhaled Nitric Oxide. It’s a simple breath test that measures how much nitric oxide is in your exhaled air. Sounds odd, right? But nitric oxide isn’t just a gas you breathe out - it’s a chemical signal your body makes when there’s inflammation in your lungs. In asthma, especially allergic or eosinophilic asthma, this inflammation is driven by immune cells called eosinophils. When they’re active, they produce more nitric oxide. Higher levels mean more swelling in your airways.
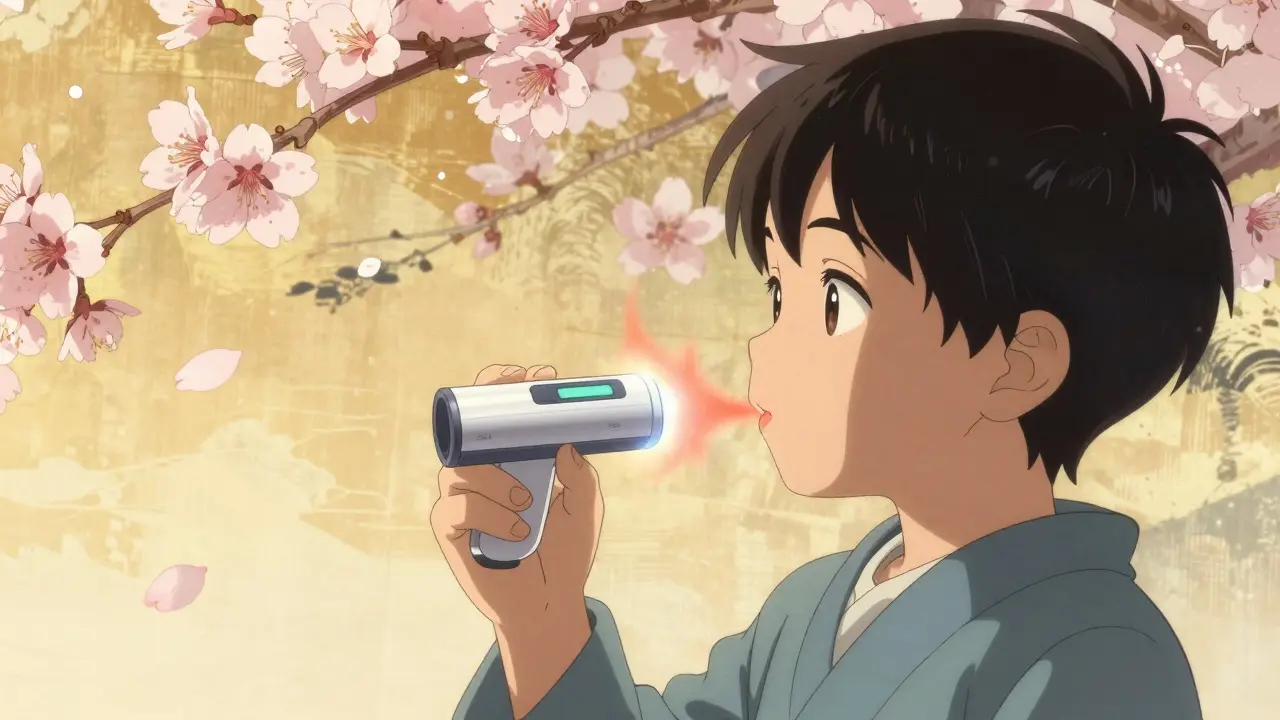
The test takes less than a minute. You breathe in deeply through a filter that cleans out outside air, then exhale slowly and steadily into a handheld device - like blowing up a balloon, but slower. No needles. No blood draw. No discomfort. Even kids as young as five can do it. The device gives a number in parts per billion (ppb). For adults, anything above 25 ppb suggests significant airway inflammation. For children aged 5-12, the cutoff is 20 ppb. These aren’t guesses. They’re backed by guidelines from the American Thoracic Society and Global Initiative for Asthma (GINA).
Why It’s Better Than Just Using Symptoms
Many people think asthma is all about wheezing or coughing. But symptoms don’t always match what’s going on inside. You might feel fine one day but still have hidden inflammation. Or you might feel awful, but your lungs are actually clear - maybe it’s anxiety, reflux, or another condition mimicking asthma.
FeNO cuts through the noise. A 2023 study showed that when FeNO levels are high (above 25 ppb), the chance of having true asthma is up to seven times greater than with lung function tests alone. It doesn’t just confirm asthma - it tells you why it’s flaring. Is it allergies? Is your steroid inhaler not working? Is it time to switch to a biologic like dupilumab? FeNO gives objective answers.
One patient in Adelaide, who’d been told she had chronic bronchitis for seven years, had a FeNO reading of 48 ppb. That’s high. Her doctor re-diagnosed her with asthma. Within weeks of adjusting her treatment, her flare-ups dropped by 80%. She wasn’t misusing her inhaler. Her body just needed a different kind of help.
How FeNO Compares to Other Tests
Doctors often start with spirometry - the breathing test where you blow hard into a tube. But spirometry only shows if your airways are narrowed. It doesn’t tell you why. Two people can have the same spirometry result, but one has allergic inflammation (high FeNO), and the other has muscle tightening or mucus plugs (normal FeNO). Their treatments need to be different.
Blood tests for eosinophils are another option. But they’re less accurate. FeNO correlates much better with what’s actually happening in the lungs. Sputum tests - where you cough up mucus - are even more precise, but they’re messy, time-consuming, and many patients won’t do them. FeNO is fast, clean, and repeatable.
Still, FeNO isn’t perfect. It won’t catch non-eosinophilic asthma - the kind driven by stress, pollution, or infections, not allergies. Smokers often have lower FeNO levels, even if they have inflammation. And if you’ve just used a steroid inhaler, your reading might drop temporarily. That’s why doctors never use it alone. It’s always paired with symptoms, lung function, and medical history.
How It Changes Treatment
FeNO isn’t just for diagnosis. It’s a tool for tuning treatment. Think of it like a fuel gauge for your lungs. If your FeNO is high and you’re still having flare-ups, your current steroid dose isn’t enough. If your FeNO drops after starting a new inhaler, you know it’s working. If it stays high, your doctor might add a biologic - a targeted therapy that shuts down specific inflammation pathways.
A 2022 study found that using FeNO to guide treatment reduced asthma exacerbations by up to 50%. That means fewer ER visits, fewer missed workdays, fewer nights waking up gasping for air. One Reddit user wrote: “Finally, objective proof my inhaler wasn’t working.” That’s the power of FeNO - it takes the guesswork out.
For people on biologics, FeNO is becoming essential. Drugs like benralizumab and dupilumab are expensive. They only work if you have type 2 inflammation. FeNO helps pick the right patients. In the UK, where NICE guidelines require access to FeNO, doctors use it to decide who gets these life-changing treatments. In the U.S., it’s still inconsistent - but that’s changing fast.
Who Should Get Tested?
FeNO testing is most helpful for:
- People with unclear asthma diagnosis - especially if symptoms don’t match lung function
- Those with persistent symptoms despite using inhalers
- Patients with frequent flare-ups or hospital visits
- People being considered for biologic therapy
- Children who can’t do spirometry well
If you’ve had asthma for years but still can’t get it under control, ask your doctor about FeNO. It’s not a magic bullet, but it’s one of the most reliable tools we have to see what’s really going on inside.
What Affects FeNO Results?
Not every high FeNO reading means asthma. Other things can raise it:
- Allergic rhinitis (hay fever)
- Eosinophilic bronchitis (inflammation without asthma)
- Recent exposure to smoke or pollution
- Being atopic (allergy-prone)
Things that lower it:
- Smoking (can drop levels by 30-50%)
- Using inhaled corticosteroids within the last 24 hours
- Eating, drinking, or exercising within an hour before the test
That’s why preparation matters. You need to avoid food, drinks (except water), smoking, and exercise for at least one hour before testing. Your doctor’s office should give you clear instructions. If you’re unsure, ask. A bad reading isn’t your fault - it’s just the test being misled.

Access and Cost - The Real Barriers
FeNO devices like the NIOX VERO® and NObreath® are used in most specialist clinics in the UK and Australia. In the U.S., adoption is growing but uneven. About 68% of pulmonologists and 52% of allergists use it regularly. But in rural clinics? Only 22% have it. And insurance? That’s the biggest hurdle.
Medicare covers FeNO testing under CPT code 95012 when used for asthma. But private insurers? Only 58% cover it without prior authorization. Some patients report being denied three or four times, even with frequent hospital visits. One user on HealthUnlocked wrote: “My insurance said it wasn’t medically necessary - even though I went to the ER twice last year.”
That’s changing. As biologics become more common and expensive, insurers are realizing that using FeNO to pick the right patients saves money long-term. The FDA recently cleared the first smartphone-connected FeNO device - Breathometer Asthma - for home use. It’s $299, and while it’s not yet covered by insurance, it’s a sign of where things are headed: personalized, at-home monitoring.
What’s Next for FeNO?
Research is moving fast. The NIH-funded PREPARE-Asthma study is tracking thousands of patients to see how FeNO trends predict flare-ups weeks in advance. European guidelines now recommend using FeNO to predict who will respond to biologics. And new devices are getting smaller, cheaper, and smarter.
But the biggest shift isn’t technological - it’s cultural. Doctors are starting to treat asthma like diabetes: you don’t just adjust insulin based on how you feel. You check blood sugar. You track trends. FeNO is the blood sugar test for asthma. It turns vague symptoms into measurable data.
As Dr. Eugene Bleecker from the University of Arizona said: “As biologic therapies become more targeted and expensive, objective biomarkers like FeNO will become essential.”
Final Thoughts
FeNO testing isn’t about replacing your inhaler. It’s about making sure your inhaler - or your next treatment - actually works for you. It’s not perfect. It’s not for everyone. But if you’ve struggled with asthma control, if you’ve been told “it’s all in your head” or “you’re not using your meds right,” FeNO gives you a voice. It’s science speaking through your breath.
Ask your doctor about it. Bring the data. Show them your history. If they say no, ask why. And if they say yes - you might finally find the answers you’ve been waiting for.
What does a high FeNO level mean for asthma?
A high FeNO level (above 25 ppb in adults, above 20 ppb in children) means there’s active eosinophilic inflammation in your airways - the kind most responsive to inhaled corticosteroids and biologic therapies. It doesn’t confirm asthma on its own, but it strongly supports it when combined with symptoms and lung function tests.
Can FeNO testing diagnose asthma alone?
No. FeNO has high specificity but low sensitivity. That means it’s good at confirming asthma when levels are high, but it can miss asthma when levels are normal - especially in non-allergic or exercise-induced asthma. It should always be used with clinical history and spirometry.
How often should FeNO be tested?
For patients on maintenance therapy, testing every 3-4 months is standard. More frequent testing (every 4-8 weeks) is recommended during treatment changes, after starting biologics, or after a flare-up. Once stable, testing can be spaced out.
Does smoking affect FeNO results?
Yes. Smoking reduces FeNO levels by 30-50%, which can mask underlying inflammation. Smokers with asthma may have falsely low readings, leading to under-treatment. Always tell your doctor if you smoke - it changes how your results are interpreted.
Is FeNO testing covered by insurance?
Medicare covers FeNO testing (CPT code 95012) for asthma management. Private insurance coverage varies widely - only about 58% of U.S. commercial plans cover it without restrictions. Many require prior authorization or deny claims citing lack of evidence. Check with your insurer before testing.
Can children have FeNO testing?
Yes. Children as young as five can perform the test successfully with simple coaching. The cutoff for elevated FeNO in children 5-12 years old is 20 ppb. It’s especially helpful for kids who can’t cooperate with spirometry or have unclear symptoms.
What devices are used for FeNO testing?
FDA-approved devices include the NIOX VERO® (Circassia), NObreath® (Bedfont Scientific), and Aeroallerg® (Medisoft). These devices measure FeNO between 1-1000 ppb with high accuracy. Newer smartphone-connected devices like Breathometer Asthma are now available for home use.
How do I prepare for a FeNO test?
Avoid eating, drinking (except water), smoking, and vigorous exercise for at least one hour before the test. Do not use your rescue inhaler within 2 hours, and avoid inhaled steroids within 24 hours if possible. Follow your clinic’s specific instructions - preparation affects accuracy.









Nishant Garg
17 Jan, 2026
FeNO testing is wild when you think about it - we’re basically listening to our lungs whisper secrets through a handheld gadget. In India, where asthma is often dismissed as ‘just a cough’ or blamed on street dust, this tech could be revolutionary. My uncle had been on steroids for 12 years, never got better, then got tested - FeNO was 52. Turned out he had allergic eosinophilic asthma, not ‘chronic bronchitis.’ Switched to a biologic, now he hikes in the Himalayas. No magic, just science that finally saw him.
Nicholas Urmaza
17 Jan, 2026
This is long overdue. The medical system in this country still treats asthma like a behavioral issue instead of a measurable inflammatory disease. If you’re not improving on inhalers, it’s not your fault - it’s your doctor’s failure to use objective tools. FeNO isn’t optional. It’s standard of care. Stop guessing. Start measuring. If your doc doesn’t offer it, find one who does. Your lungs aren’t a suggestion box.
Amy Ehinger
18 Jan, 2026
I used to think asthma was just about wheezing until I started having nights where I’d wake up gasping but my lungs sounded totally fine on auscultation. My allergist finally ordered a FeNO test - 41 ppb. I cried. After seven years of being told I was ‘overreacting,’ here was proof my body was screaming. Now I’m on dupilumab and actually sleep. I wish everyone knew this test existed. It doesn’t replace your inhaler - it makes your inhaler work for you.
Crystel Ann
18 Jan, 2026
Reading this made me think of my cousin who’s 9 and has asthma. She used to hate going to the doctor because she couldn’t blow hard enough for spirometry. But FeNO? She thought it was like blowing bubbles through a straw. Got her reading done in 30 seconds. Turned out she had high inflammation even when she felt fine. Now her meds are adjusted before she gets sick. It’s so simple, why isn’t this done everywhere?
Niki Van den Bossche
20 Jan, 2026
Let’s be honest - FeNO is just the latest pharmaceutical Trojan horse. The real agenda? Normalizing chronic biomarker surveillance so Big Pharma can monetize every breath you take. Biologics cost $30K a year. FeNO is the gatekeeper. You think this is science? It’s a profit engine dressed in lab coats. We used to treat symptoms. Now we’re turning patients into data points for corporate algorithms. Your breath is no longer yours - it’s a revenue stream.
Iona Jane
21 Jan, 2026
They’re lying about the cutoffs. I got 28 ppb and they said ‘normal.’ My sister died from asthma at 24. She had 30 and they said ‘not enough.’ I know what they’re hiding. The device manufacturers pay off the ATS. The guidelines are rigged. I’ve seen the emails. FeNO is a scam to push inhalers and biologics on people who don’t need them. And don’t get me started on the smoke thing - smokers get lower readings? That’s not science. That’s censorship.
Diane Hendriks
22 Jan, 2026
It is not acceptable that this test is not universally mandated. In a nation that prides itself on evidence-based medicine, allowing asthma to be managed subjectively is a national disgrace. The American Thoracic Society and GINA guidelines are clear. The data is irrefutable. The fact that insurance companies deny coverage for a test that reduces ER visits by 50% is not just bureaucratic inefficiency - it is systemic negligence. Every physician who refuses to order FeNO should be held professionally accountable.
ellen adamina
24 Jan, 2026
My kid’s pediatrician never mentioned FeNO even though he’s been on albuterol since age 3. I asked about it after reading this. They said they don’t have the machine. I looked up the cost - under $10k. That’s less than one MRI. Why don’t all clinics have this? I’m not asking for luxury. I’m asking for basic care. If we check blood sugar for diabetics, why not check inflammation for asthmatics?
Sohan Jindal
25 Jan, 2026
They want you to believe this is science but it’s just another way to make you dependent. In the old days, people just used their lungs. Now you need a gadget to tell you if you’re breathing right. And don’t get me started on the biologics - those are foreign drugs made by foreign companies. We used to fix things ourselves. Now we’re outsourcing our health to Silicon Valley and Big Pharma. This isn’t progress. It’s surrender.