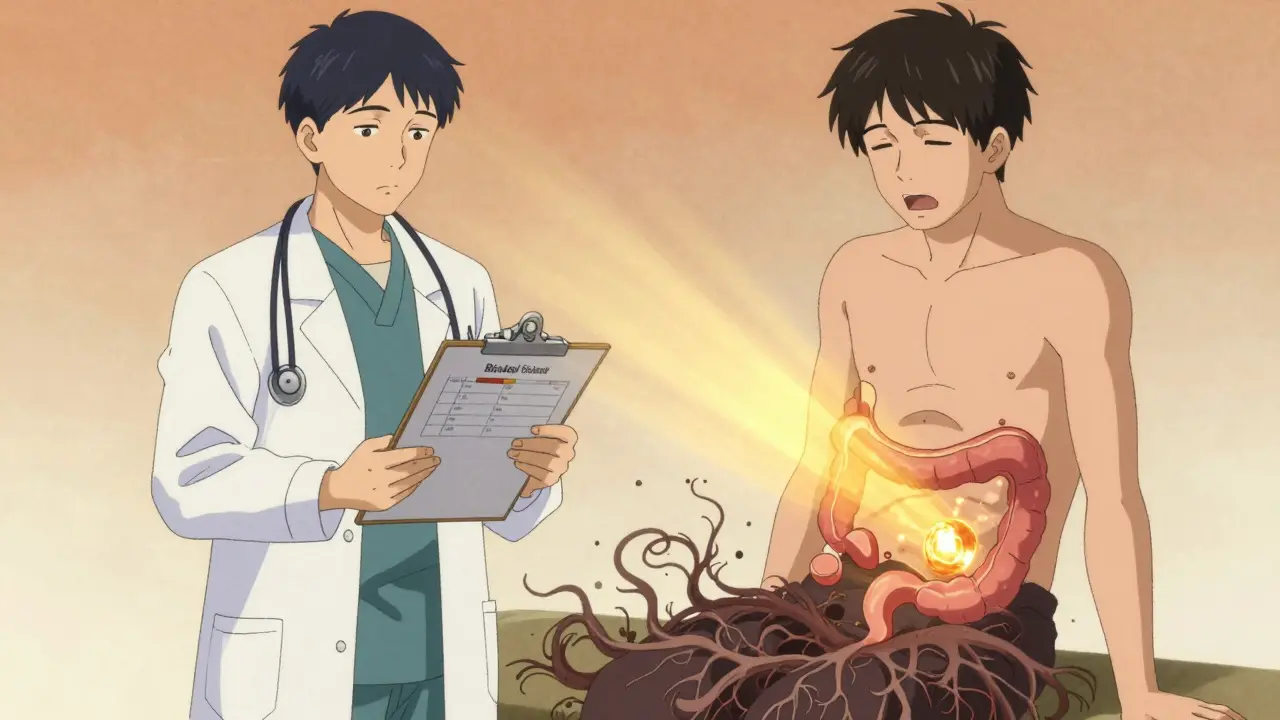
When you start taking opioids for chronic pain, you’re told about the risks: drowsiness, nausea, addiction. But few warn you about the one side effect that can make daily life unbearable - opioid-induced constipation. It doesn’t go away. It doesn’t get better with time. And if you don’t treat it early, it can force you to stop your pain medication altogether.
Up to 95% of people on long-term opioids develop this problem. That’s not rare. That’s the rule. And yet, studies show only 15-30% of patients get the right treatment from the start. Why? Because doctors still think it’s just "normal constipation" - and treat it like it is.
But here’s the truth: opioid-induced constipation (OIC) isn’t the same as what you get from eating too much cheese or skipping your morning coffee. It’s a different beast. Opioids lock up the muscles in your gut. They slow down the movement of food. They dry out your stool. And they stop your body from producing the fluids needed to pass it. No amount of prunes or bran cereal will fix that.
Why Fiber Won’t Help - and Might Make It Worse
You’ve probably heard the advice: "Eat more fiber. Drink more water. Exercise." That works for general constipation. But with OIC, it backfires.
When opioids shut down gut movement, fiber doesn’t move through your system. It sits there. Ferments. Swells. Causes bloating, gas, and even dangerous fecal impactions. A 2023 review in the Taylor & Francis Journal of Neurogastroenterology found that 25-40% of OIC patients get worse when they increase fiber intake. The American Pain Society updated its guidelines in 2020 to explicitly warn against high-fiber diets for OIC.
So if you’re on opioids and your doctor told you to eat 30 grams of fiber a day - stop. That advice could be hurting you.
What Actually Works: First-Line Treatments
For OIC, the first step isn’t fancy drugs. It’s simple, cheap, and backed by solid science: osmotic laxatives.
Polyethylene glycol (PEG), sold as Miralax or Macrogol, is the gold standard. Take 17-34 grams daily. It pulls water into your colon without irritating the gut. Unlike stimulant laxatives, it doesn’t cause cramping or dependency. Studies show it works in about 50% of OIC cases - better than most alternatives.
Stimulant laxatives like senna or bisacodyl are second-choice. They force your bowels to contract. They work faster - often within 6-12 hours. But they can cause cramps. And if you use them long-term, your colon can lose its natural rhythm. Use them short-term, or if PEG doesn’t cut it.
Here’s what to do when you start opioids:
- Ask your doctor to assess your bowel function before you begin - use the Bristol Stool Scale or an OIC Severity Scale.
- Start PEG (17g/day) on day one - don’t wait for symptoms.
- Drink at least 2 liters of water daily. Opioids dehydrate you; water counters that.
- Track your bowel movements weekly. If you’re going less than three times a week, adjust your dose.
Most patients see improvement within a week. If not, it’s time to move to step two.
Prescription Options When Laxatives Fail
Half of OIC patients don’t respond to over-the-counter laxatives. That’s not your fault. It’s the biology.
That’s where peripherally acting μ-opioid receptor antagonists (PAMORAs) come in. These are the only drugs designed specifically to undo opioid effects in the gut - without touching pain relief in your brain.
There are three main ones:
- Methylnaltrexone (Relistor®): Injected under the skin. Works in as little as 30 minutes. Used mostly for patients in palliative care. Cost: $800-$1,200/month. Side effects: injection-site pain (47% of users), dizziness.
- Naloxegol (Movantik®): A daily pill. Approved for chronic non-cancer pain. Takes 24-48 hours to work. Side effects: abdominal pain (25%), nausea (15%). Cost: $500-$900/month.
- Naldemedine (Symcorza®): Also a daily pill. FDA-approved for adults and kids over 12 since March 2023. Works faster than naloxegol. Side effects: mild diarrhea (18%), stomach pain (38%). Cost: $600-$1,000/month. Patient ratings average 6.8/10 - highest among PAMORAs.
These drugs aren’t perfect. But they work. Clinical trials show 40-50% of patients have a meaningful improvement in bowel function - compared to 25-30% with placebo.
There’s also lubiprostone (Amitiza®). It’s a chloride channel activator that draws fluid into the intestines. It works for OIC, but it’s not ideal. It was originally approved only for women because early trials didn’t include enough men. Later data showed it works just as well in men - but the label hasn’t changed. Side effects? Nausea in 30% of users. Diarrhea in 15-20%. And it can’t be used with diuretics.
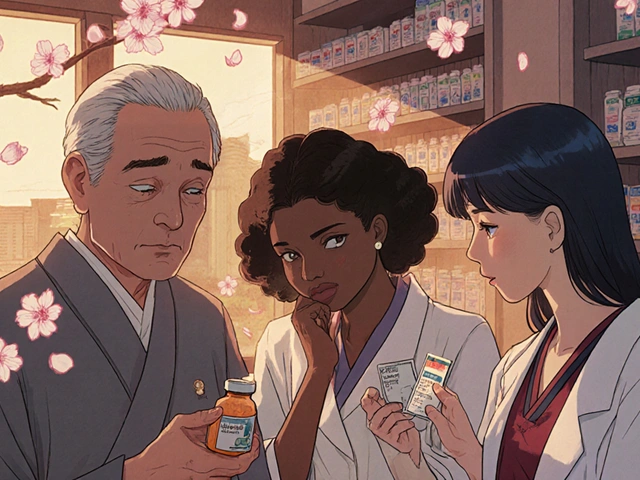
The Cost Problem
PAMORAs are expensive. Insurance often won’t cover them unless you’ve tried and failed at least two laxatives first. That’s called "step therapy." And it’s a problem.
Patients on Reddit’s r/ChronicPain forum say they’ve spent months trying Miralax, senna, and fiber supplements - only to end up with severe impaction before their insurer approves a PAMORA. One user wrote: "I had to go to the ER because I couldn’t poop for 10 days. Then they approved the shot. Took 3 hours to work. I cried. I was so relieved. But why did I have to suffer to get help?"
Even with insurance, co-pays can be $100-$300 a month. Without it? You’re looking at $1,000 a month. That’s not sustainable for most.
What Patients Are Really Doing
Real people aren’t waiting for doctors to fix this. They’re self-managing.
On Drugs.com, 89% of comments about OIC mention Miralax. Many users double or triple the dose. Some mix it with prune juice or coffee. Others skip doses when they feel fine - then pay for it later.
A 2022 survey in Pain Management Nursing found that 73% of patients have stopped at least one OIC treatment because it didn’t work or caused side effects. Only 19% of general practitioners feel confident managing OIC. But 80% of nurses say a simplified treatment algorithm - just three steps - would help them do their job better.
That’s the gap. Patients are desperate. Providers are overwhelmed. And the system isn’t built to catch this early.

What You Can Do Right Now
If you’re on opioids and constipated:
- Stop adding fiber. Seriously. It’s not helping.
- Start polyethylene glycol (PEG) at 17g/day. Increase to 34g if no results in 5 days.
- Drink water. At least 2 liters. More if you’re active or in hot weather.
- Track your bowel movements. Use a simple calendar. Note stool form (Bristol Scale: 1-7). Aim for 3-5 soft, easy-to-pass stools per week.
- If you’re not improving after 7-10 days, ask your doctor about PAMORAs. Say: "I’ve tried standard laxatives. I need a drug that targets opioid effects in the gut. What do you recommend?"
- If cost is an issue, ask about patient assistance programs. All three PAMORAs have them.
And if you’re a caregiver or family member - don’t wait for your loved one to complain. Ask them: "How often are you going?" "Is it painful?" "Are you taking anything for it?"
The Bigger Picture
OIC isn’t just a nuisance. It’s a treatment barrier. Studies show 30-40% of patients reduce or stop their opioid dose because of constipation - even when their pain is still severe. That means they’re in more pain, not less.
That’s why the FDA now requires opioid manufacturers to include OIC education in their Risk Evaluation and Mitigation Strategies (REMS). That’s why major hospitals are rolling out standardized OIC protocols. And that’s why the global OIC treatment market is projected to hit $3.4 billion by 2028.
But progress is slow. In community clinics, only 22-35% of doctors use any formal OIC assessment tool. Meanwhile, 100 million Americans get opioid prescriptions every year. That’s tens of millions of people silently suffering.
It doesn’t have to be this way. OIC is preventable. Treatable. Manageable. But only if you know what to do - and when to ask for help.
You don’t have to choose between pain relief and dignity. You just need the right tools - and the courage to speak up.
Can I just use over-the-counter laxatives for opioid-induced constipation?
Yes - but only at first. Osmotic laxatives like polyethylene glycol (Miralax) work for about half of patients. Stimulant laxatives like senna can help short-term. But if you’ve tried these for 7-10 days and still aren’t having regular bowel movements, they’re not enough. OIC has a unique cause - opioids slowing your gut - and standard laxatives don’t fix that. You’ll need a prescription drug like a PAMORA.
Why is fiber bad for opioid-induced constipation?
Opioids stop your gut from moving. Fiber doesn’t move either - it just sits there, swells, and ferments. That causes bloating, gas, and can lead to fecal impaction. Unlike regular constipation, where fiber helps, OIC is caused by slow movement, not dry stool. Adding fiber makes the problem worse for 25-40% of patients. Guidelines now advise against high-fiber diets for OIC.
What are PAMORAs and how do they work?
PAMORAs - peripherally acting μ-opioid receptor antagonists - block opioid effects in your gut without crossing the blood-brain barrier. That means they fix constipation but don’t interfere with pain relief. Examples include methylnaltrexone (Relistor®), naloxegol (Movantik®), and naldemedine (Symcorza®). They’re taken as injections or pills and work in hours to days. Response rates are 40-50%, much higher than standard laxatives.
Are PAMORAs covered by insurance?
Often, but not always. Most insurers require you to try and fail at least two over-the-counter laxatives first. This is called "step therapy." Some also require documentation from your doctor that your constipation is severe and linked to opioids. Patient assistance programs are available for all three major PAMORAs - ask your pharmacist or the drug manufacturer.
How long does it take for OIC treatments to work?
It depends. Polyethylene glycol usually works in 1-3 days. Stimulant laxatives like senna can work in 6-12 hours. PAMORAs vary: methylnaltrexone injections work in 30 minutes to 4 hours. Naloxegol and naldemedine pills take 24-48 hours. Lubiprostone takes 1-2 days. If nothing works after 7 days, talk to your doctor about switching or adding another treatment.
Can opioid-induced constipation lead to serious complications?
Yes. Untreated OIC can lead to fecal impaction - where stool becomes so hard and large it can’t pass. This can cause bowel obstruction, perforation, or infection. In severe cases, it requires emergency surgery. Chronic OIC also reduces quality of life, causes depression, and leads many patients to stop their pain medication - leaving them in more pain. Early treatment prevents these outcomes.
Is there a new treatment for OIC coming soon?
Yes. A combination pill of naloxone and polyethylene glycol is in Phase III trials and could be approved by mid-2024. This would combine the gut-targeted action of naloxone with the gentle osmotic effect of PEG - potentially offering better results with fewer side effects. It’s designed to be cheaper and easier to use than current PAMORAs.
If you’re managing OIC, remember: you’re not alone. The system is broken, but the solutions exist. Speak up. Track your symptoms. Ask for the right tools. Your pain doesn’t have to come with a prison of constipation.










josue robert figueroa salazar
26 Dec, 2025
Fiber is the enemy. Stop listening to your grandma. PEG is the only thing that works.
david jackson
28 Dec, 2025
I’ve been on oxycodone for six years now, and I swear I’ve tried everything - prunes, flaxseed, enemas, yoga, even that weird ‘abdominal massage’ video on YouTube. Nothing worked until I finally pushed for Movantik. My doctor acted like I was asking for heroin. Took three months of begging, three letters from my pain nurse, and a trip to the ER with a 10-day impaction before they approved it. Now I’m going every day. No more bloating. No more pain. But why does it have to be this hard? Why does my body’s most basic function have to be a battle royale just to get a prescription? I’m not asking for magic. I’m asking for dignity.
christian ebongue
29 Dec, 2025
PEG 17g/day? lol. Try 34g. And drink water like you’re trying to fill a swimming pool. Also, stop calling it 'constipation' - it's opioid-induced gut paralysis. Semantics matter.
jesse chen
31 Dec, 2025
I just want to say… thank you. This post saved me. I was about to quit my meds because I couldn’t poop without crying. I started PEG yesterday. I’ve already had two soft bowel movements. I didn’t think it was possible. Please, if you’re reading this and you’re suffering - don’t suffer in silence. Ask for help. You deserve to live without this.
Joanne Smith
1 Jan, 2026
So let me get this straight… we’re telling people to stop eating fiber, but also to spend $800/month on a drug that makes you dizzy and gives you injection-site pain? And the system makes you suffer for months before they’ll even *consider* it? Yeah. That’s not healthcare. That’s a hostage situation with a pharmacy receipt.
Prasanthi Kontemukkala
1 Jan, 2026
I appreciate how clear and practical this is. As a nurse in a rural clinic, I see so many patients who are told to 'just eat more apples.' I’ve started handing out printed copies of this to my patients. It’s a game-changer. Thank you for writing this - and for not sugarcoating the cost issue. We need more voices like yours.
Lori Anne Franklin
1 Jan, 2026
i started peg like u said and omg it worked?? i thought i was gonna die. also i mixed it with orange juice bc the taste is gross. and yes i know i’m not supposed to but i did. and i’m still alive. thanks for this.
Bryan Woods
3 Jan, 2026
The clinical data presented here is compelling. However, the systemic barriers to access - particularly step therapy requirements - remain a critical flaw in patient care. Until insurance policies align with evidence-based guidelines, patient suffering will persist as a structural issue, not an individual failure.