Medication Timing Advisor
How Timing Affects Your Medication
Your body's natural clock affects how medications work. Taking the right dose at the wrong time can reduce effectiveness or increase side effects.
Optimal Timing Recommendation
Practical Tip:
What if taking your pill at 7 a.m. instead of 10 p.m. could make it work better-or even stop it from making you sick? It’s not magic. It’s chronotherapy: using your body’s natural 24-hour clock to time your meds for maximum benefit and minimum side effects.
Why Timing Matters More Than You Think
Your body doesn’t run on a flat line. It pulses. Heart rate rises in the morning. Liver enzymes peak at night. Blood pressure drops during sleep. These rhythms affect how your body absorbs, breaks down, and gets rid of drugs. Take a medication at the wrong time, and you might get more side effects-or less help. For example, statins-medications that lower cholesterol-work best when taken at night. That’s because your liver makes most of its cholesterol while you’re asleep. Taking them in the evening boosts their effect by 15-20% compared to morning doses. Same dose. Same pill. Just better timing. Insulin is another big one. If you take your fast-acting insulin too early before a meal, your blood sugar can crash. Too late, and it spikes. A 15-minute window can mean the difference between feeling fine and ending up in the ER.High-Risk Meds That Can’t Wait
Not all medications are created equal when it comes to timing. Some are forgiving. Others? Not even close. Anticoagulants like warfarin need precise timing. A study found that mistimed doses increased bleeding risk by up to 37%. Why? Because the enzymes that break down these drugs swing wildly throughout the day. Take it at 8 a.m. one day and 8 p.m. the next, and your blood’s clotting ability can go off-kilter. Chemotherapy drugs are even stricter. Deviating from the scheduled time by more than 30 minutes can cut effectiveness by 15-20%. In cancer treatment, that’s not just inconvenient-it’s dangerous. Even common drugs like beta-blockers for heart conditions benefit from timing. One ICU team saw post-surgery atrial fibrillation drop by nearly 40% after switching to strict evening dosing. The heart’s rhythm is most unstable in the early morning. Matching the drug’s peak effect to that window made a measurable difference.When Timing Doesn’t Matter (Much)
Before you start stressing over every minute, know this: not every pill needs a stopwatch. Medications like hydrochlorothiazide (a water pill for high blood pressure) can be taken within a 12-hour window without losing effectiveness. Same with many antibiotics for simple infections. Your body can handle some flexibility. But here’s the catch: even “forgiving” meds can cause problems if taken at the wrong time. Take a diuretic at night, and you’ll be up every two hours to pee. That’s not a side effect of the drug-it’s a side effect of bad timing. The real issue isn’t just whether the drug works. It’s whether it causes discomfort, disrupts sleep, or creates new risks. Timing isn’t just about potency. It’s about quality of life.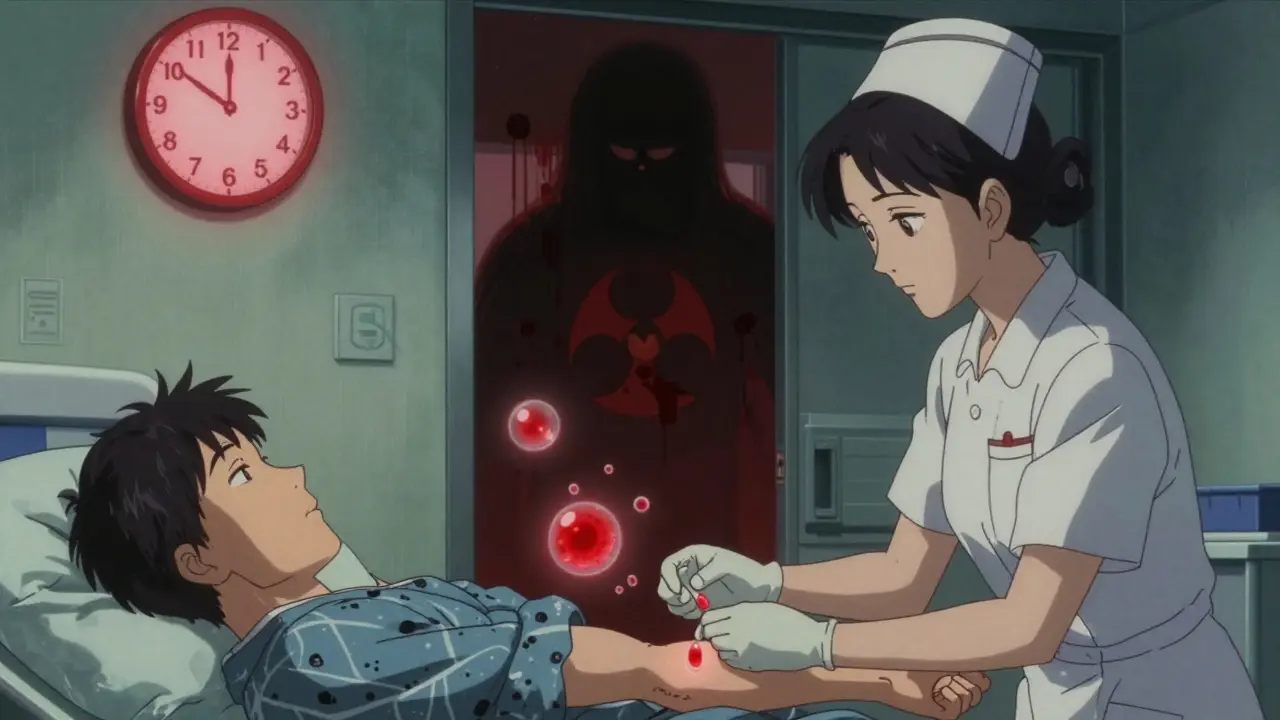
Why Hospitals Get It Right-And Why You Don’t
In hospitals, nurses follow strict protocols. Barcode scanners, timed charts, and computer alerts help ensure meds are given at the right hour. But even then, errors happen. A 2022 report found that 48-53% of IV medication doses had timing errors-often because of interruptions during rounds. At home, it’s worse. A survey of 1,200 patients found 68% couldn’t stick to their prescribed timing. Why? Work schedules. Forgetfulness. Lack of clear instructions. One nurse on Reddit said, “We’re lucky to get within 30 minutes of scheduled times.” That’s not just a problem-it’s a public health gap. People with low health literacy are 74% more likely to mess up timing. If your doctor says “take it at bedtime,” but you’re not sure what that means, you’ll wing it. And winging it with meds can be risky.How to Get Your Timing Right
You don’t need a PhD to get this right. Here’s how to start:- Ask your pharmacist: “Is there a best time to take this?” Don’t assume it doesn’t matter.
- Check if your med has a known chronotherapeutic window. Statins? Night. Blood pressure meds like ACE inhibitors? Bedtime (studies show they reduce heart events by 29% when taken at night).
- Use alarms. Not just phone alerts-physical pill dispensers with lights or sounds. They cut timing errors by up to 28%.
- Keep a simple log: write down when you took each pill for a week. You might spot patterns you didn’t know existed.
- If you miss a dose, don’t double up. Call your doctor or pharmacist. Some meds can be taken late; others shouldn’t be taken at all if it’s too close to the next dose.












Roshan Joy
10 Jan, 2026
Been taking my statins at night since my doc mentioned this last year. No more muscle aches in the morning. Also, my sleep’s way better-no more midnight bathroom marathons. Simple fix, huge difference.
Also, using a pill dispenser with a light. It beeps like a tiny robot but it works.
Jennifer Littler
12 Jan, 2026
Chronotherapy is underutilized in primary care because most clinicians aren’t trained in circadian pharmacokinetics. The NIH has published multiple meta-analyses on time-dependent bioavailability, yet EHR systems rarely flag it. We’re treating pharmacodynamics like it’s static when it’s profoundly rhythmic.
Also, the 29% reduction in cardiovascular events with nighttime ACE inhibitors? That’s not a nuance-it’s a clinical imperative.
Jason Shriner
12 Jan, 2026
so like… if i take my blood pressure med at 11pm instead of 10pm… am i basically doing a 2 hour time travel to the future where my heart explodes?
just asking for a friend. who is me. who forgot again.
Vincent Clarizio
14 Jan, 2026
Let’s be real-this isn’t just about timing. This is about the entire medical industrial complex refusing to acknowledge that the human body is not a vending machine. We don’t just drop a pill in and get a predictable outcome. Our biology is a symphony, not a spreadsheet.
Warfarin isn’t just ‘taken at night’-it’s taken when your VKORC1 enzyme is most receptive, which is dictated by your circadian rhythm, which is dictated by your light exposure, which is dictated by your screen time, which is dictated by your depression, which is dictated by your job, which is dictated by capitalism.
And yet the system wants you to take it at 8 p.m. like it’s a TikTok challenge. Meanwhile, your liver is screaming in a language no one bothered to learn.
They’ll slap a ChronoCare alert on your chart in 2025, but they won’t fix the fact that you’re working two jobs and your sleep schedule is a meme.
Alex Smith
14 Jan, 2026
Actually, I’ve seen this play out in my dad’s care-he’s on warfarin and was taking it randomly until his pharmacist sat him down with a chart. Now he takes it at 6 p.m. sharp, uses a pill organizer with a timer, and hasn’t had a single INR spike in 18 months.
It’s not rocket science. It’s just… consistency. And someone actually explaining why it matters. Most docs say ‘take it at bedtime’ and walk away. That’s not care, that’s a suggestion with a prescription.
Also, the 28% reduction in timing errors with physical dispensers? That’s a no-brainer. Why aren’t these things covered by insurance?
Adewumi Gbotemi
15 Jan, 2026
Here in Nigeria, many people just take pills when they remember, or when they feel sick. No alarms. No charts. But I told my uncle about the night statins thing-he now takes his at 9 p.m. and says his legs don’t ache anymore. Small change, big difference.
Maybe we need more community health workers to explain this. Not just doctors.
Michael Patterson
16 Jan, 2026
Ugh. Another ‘science’ article that sounds smart but ignores reality. Most people don’t even know what ‘chronotherapy’ means. You think grandma with dementia is gonna remember to take her meds at 6 p.m. because some study says so? She’ll take it with her coffee at 7 a.m. and then complain about the diarrhea.
Also, ‘timing critical’ alerts? Yeah, right. My pharmacy app still thinks I take metformin at 8 a.m. when I’ve been taking it at 10 p.m. for 3 years. It doesn’t even ask.
Matthew Miller
18 Jan, 2026
This is pure pseudoscience wrapped in a pretty infographic. ‘Liver enzymes peak at night’? Name one peer-reviewed study that proves that’s universally true across all demographics. And ‘statins work better at night’? That’s from a 2006 trial with 800 patients. We’ve had 18 years of bigger, better studies since.
Meanwhile, people are dying because they’re overcomplicating their meds instead of just taking them consistently. Timing is a luxury for people who don’t work swing shifts or have kids who wake up at 4 a.m.
Stop gaslighting patients with ‘biological rhythms’ and fix the system that makes adherence impossible.
Madhav Malhotra
18 Jan, 2026
In India, we call this ‘din ka samay’-the time of day. Our grandmas always said, ‘take the bitter pill after dinner, not before sleep.’ Turns out they were right.
My aunt takes her BP med after dinner, and her morning headaches vanished. No doctor told her-she just listened to her body.
Maybe the science is catching up to what people have always known.