Facial flushing isn’t just blushing after a spicy meal or a heated conversation. For millions of people, it’s the first sign of something deeper-rosacea. This isn’t a temporary redness that fades after a few minutes. It’s persistent, unpredictable, and often accompanied by burning, bumps, and visible blood vessels. And while it’s not dangerous, it can be deeply frustrating. Many people spend years thinking they have sensitive skin, acne, or just bad luck with sun exposure-until they learn it’s rosacea.
What Exactly Is Rosacea?
Rosacea is a chronic skin condition that mainly affects the central face: cheeks, nose, forehead, and chin. It’s not caused by poor hygiene, alcohol abuse, or stress alone-though those can make it worse. It’s a complex mix of genetics, immune system overreactions, and overactive blood vessels. About 75% of people with rosacea first notice flushing-sudden, intense redness that lasts longer than normal blushing. These episodes can be triggered by simple things: a hot coffee, a walk in the sun, or even a strong emotion.Over time, that flushing turns into permanent redness. The skin doesn’t calm down. Blood vessels become visible, looking like thin red lines under the surface. Then, for about half of those affected, small red bumps and pus-filled pimples appear-often mistaken for acne. But unlike acne, rosacea doesn’t cause blackheads. And unlike acne, it doesn’t respond to typical spot treatments.
Men are less likely to be diagnosed, but when they are, the condition tends to be more severe. About 5-10% of men with rosacea develop rhinophyma-a thickening of the skin on the nose. Women make up about 60% of cases, but the emotional toll is high for everyone. Studies show that 40-60% of people with rosacea feel anxious, embarrassed, or even depressed because of how their skin looks.
Why Does Flushing Happen?
Normal blushing is a quick, emotional response. Rosacea flushing is different. It’s triggered by environmental factors and lasts longer-sometimes hours. Common triggers include:- Hot drinks (over 60°C / 140°F)
- Alcohol, especially red wine
- Spicy foods with capsaicin
- UV exposure (UV index above 3)
- Extreme cold or heat (below 0°C or above 32°C)
- Stress or strong emotions
These triggers cause blood vessels in the face to overreact, dilating too much and too often. Dermoscopy-a tool dermatologists use-shows these vessels as tiny red lines, 0.05 to 0.2mm wide. In people with rosacea, the redness on the face is 15-25% more intense than in unaffected skin, measured by standardized photography.
And it’s not just the skin. About half of all rosacea patients also have eye symptoms-dryness, burning, redness, or sensitivity to light. This is called ocular rosacea, and it’s often overlooked. If your eyes feel irritated along with your face, it’s worth mentioning to your doctor.
Topical Antibiotics: The First-Line Defense
When bumps and pimples show up, topical antibiotics become the go-to treatment. They don’t fight infection the way antibiotics do for a sore throat. Instead, they calm inflammation and reduce the population of Demodex mites-tiny creatures that live on everyone’s skin but multiply in rosacea-prone areas.Three topical treatments are most commonly used:
- Metronidazole 0.75% gel (Rozex®): Approved in 1985, it’s the oldest option. Studies show it reduces inflammatory lesions by 60-70% after 6-9 weeks of twice-daily use.
- Ivermectin 1% cream (Soolantra®): Approved in 2014, it’s now the most effective. A 2019 study found it reduced bumps and pimples by 76% in 12 weeks-better than metronidazole.
- Azelaic acid 15% gel (Finacea®): Not an antibiotic, but works similarly. It reduces inflammation and kills bacteria without antibacterial properties. It’s effective in 68-73% of cases after 15 weeks.
Here’s how they compare:
| Treatment | Active Ingredient | Reduction in Lesions | Time to Notice Improvement | Common Side Effects |
|---|---|---|---|---|
| Ivermectin 1% | Ivermectin | 76% | 4-8 weeks | Burning (22%), dryness (18%) |
| Metronidazole 0.75% | Metronidazole | 60-70% | 6-9 weeks | Burning (15%), dryness (12%) |
| Azelaic Acid 15% | Azelaic acid | 68-73% | 8-15 weeks | Stinging (20%), redness (10%) |
Even though ivermectin works better, metronidazole is still often recommended first for people with very sensitive skin. It’s gentler. Azelaic acid is a good alternative for those who don’t respond to antibiotics or prefer non-antibiotic options.

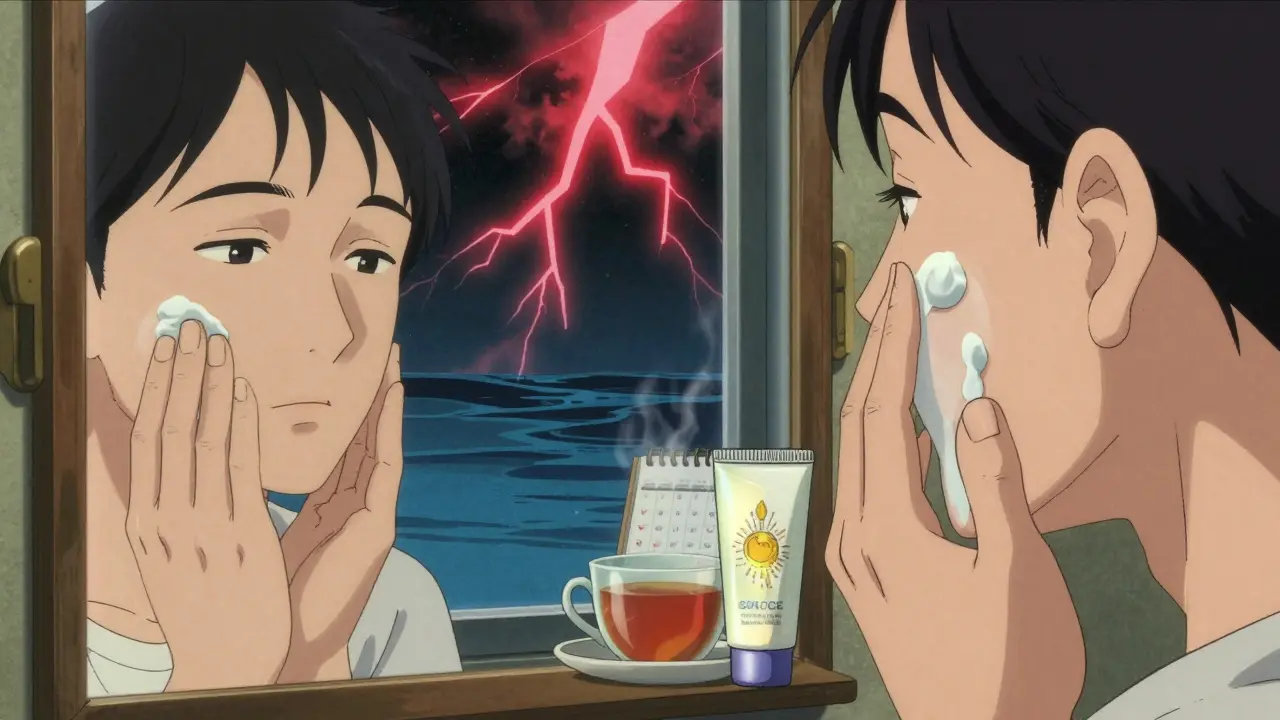
What You Need to Know Before Starting Treatment
Topical treatments don’t work overnight. Most people don’t see results until after 4-8 weeks. Full improvement can take up to 16 weeks. That’s a long time to wait when your face is already red and angry. Many patients quit too soon.Only 40-50% of people stick with their treatment past three months. Why? Because it feels slow. Because their skin stings at first. Because it’s expensive-up to $350 a year without insurance.
Here’s how to make it work:
- Start slow. Do a patch test on your jawline for 3 days before applying to your whole face.
- Use a pea-sized amount. Spread it gently over your entire face-not just the red spots.
- Wait 15-20 minutes after washing your face before applying.
- Apply to slightly damp skin. This reduces stinging without washing off the medication.
- Don’t stop if it gets worse at first. Many people report a flare-up in the first two weeks. That’s normal. Stick with it.
Side effects are usually mild: burning, dryness, or redness. Serious reactions are rare-under 1% of users. If you get severe irritation, swelling, or a rash, stop and call your doctor.
Antibiotics Alone Aren’t Enough
Topical antibiotics are great for bumps and pimples. But they do almost nothing for facial flushing or the constant redness. That’s where other treatments come in.For persistent redness, dermatologists often add:
- Brimonidine 0.33% gel (Mirvaso®): Temporarily tightens blood vessels to reduce redness for up to 12 hours.
- Oxymetazoline 1% cream (Rhofade®): Works similarly, with effects lasting up to 12 hours.
These aren’t cures. They’re temporary fixes. Used daily, they help manage appearance but don’t treat the root cause. That’s why experts say treatment should be holistic.
Dr. Linda Stein Gold, a leading dermatologist, says: “Ivermectin has become our first-line recommendation for papulopustular rosacea due to its dual anti-inflammatory and anti-Demodex activity.”
But Dr. Hilary Franck warns: “Topical antibiotics should be part of a comprehensive strategy-trigger avoidance, gentle skincare, and sun protection. Monotherapy rarely clears rosacea completely.”
Skincare and Lifestyle: The Missing Pieces
You can apply the best cream in the world, but if you’re still drinking red wine every night or skipping sunscreen, your skin won’t improve.Here’s what works:
- Use a gentle cleanser. Look for fragrance-free, non-foaming formulas with a pH between 5.5 and 7.0.
- Wear mineral sunscreen daily. Zinc oxide (10-20%) is the best choice-it doesn’t irritate sensitive skin.
- Moisturize with ceramides. These help repair the skin barrier, which is often damaged in rosacea.
- Keep a trigger diary. Write down what you ate, drank, or did before each flare-up. Patterns emerge over time.
- Avoid harsh products. No alcohol-based toners, physical scrubs, or strong acids like glycolic or salicylic acid.
People who combine medication with these habits report much better results. A 2023 survey found that 78% of dermatologists now recommend combining topical antibiotics with other treatments from day one.
What If It Doesn’t Work?
If you’ve been using your topical treatment for 8 weeks and see less than 25% improvement, it’s time to reassess. You might need:- A different medication
- Oral antibiotics like doxycycline (low-dose, for anti-inflammatory effect)
- Laser therapy to reduce visible blood vessels
- Or a referral to a specialist
Don’t wait. Rosacea doesn’t get better on its own. And the longer you wait, the more likely it is to progress.
Looking Ahead
The global rosacea treatment market is growing fast-projected to hit $2.74 billion by 2030. New treatments are on the horizon. One promising option is a combination cream with ivermectin and hydrocortisone, currently in Phase III trials. Early results show 85% lesion reduction-better than ivermectin alone.But even with new drugs, the foundation of treatment won’t change: identify your triggers, protect your skin, and use the right medication consistently.
Topical antibiotics aren’t magic. But for millions of people, they’re the key to regaining control. Not over night. Not perfectly. But enough to feel like yourself again.
Can rosacea be cured?
No, rosacea cannot be cured. But it can be managed very effectively. With the right combination of medication, skincare, and trigger avoidance, most people can keep their symptoms under control for years, even decades. The goal isn’t perfection-it’s consistency.
Do topical antibiotics make rosacea worse at first?
Yes, some people experience a temporary flare-up in the first 1-2 weeks. This is called a “purging” phase and is common with many acne and rosacea treatments. It doesn’t mean the treatment isn’t working-it means your skin is adjusting. If irritation is severe or lasts longer than 3 weeks, talk to your doctor.
Is ivermectin better than metronidazole?
Yes, in terms of effectiveness. Ivermectin reduces lesions by 76% compared to 60-70% for metronidazole. But metronidazole is gentler on sensitive skin and costs less. Many doctors start with metronidazole and switch to ivermectin if results aren’t good enough after 8-12 weeks.
Can I use makeup with topical antibiotics?
Yes, but wait at least 15 minutes after applying your medication before putting on makeup. Use mineral-based, fragrance-free products labeled “non-comedogenic.” Avoid heavy foundations-they can clog pores and trap heat, worsening flushing.
How long do I need to use topical antibiotics?
Most people use them long-term, often for months or years. Rosacea is chronic, so treatment is usually maintenance, not a short course. Some people can reduce frequency after 6-12 months of clear skin, but stopping completely often leads to a return of symptoms.
If you’re struggling with rosacea, you’re not alone. Millions of people manage it every day. The key isn’t finding a miracle cure-it’s building a routine that works for you. Be patient. Be consistent. And don’t give up before the treatment has time to work.









Sam Davies
10 Jan, 2026
So let me get this straight-we’re prescribing antiparasitic cream for a condition caused by… mites? Next they’ll tell us to scrub our faces with garlic and call it ‘ancient Indian wisdom.’
Madhav Malhotra
11 Jan, 2026
Been dealing with this for 8 years. Ivermectin saved my life, honestly. But the burning? Oh man. First two weeks felt like I’d rubbed chili paste on my cheeks. Now I can go out without sunglasses indoors. Worth it.
Priya Patel
13 Jan, 2026
Same! I started with metronidazole, hated the stinging, switched to ivermectin, and now I wear makeup without feeling like I’m hiding a crime scene. Also, mineral sunscreen is non-negotiable. Zinc oxide is my BFF.
Jason Shriner
14 Jan, 2026
so… uhh… i tried ivermectin… and my face looked like a angry tomato for 10 days… then it got better? idk man. maybe its the tea i drink. or my cat. or the moon. 🌕
Vincent Clarizio
16 Jan, 2026
Let’s be real-this isn’t just a skin condition. It’s a metaphysical mirror. Every flush, every red patch-it’s your soul screaming, ‘I’m overwhelmed!’ The Demodex mites? They’re not just arthropods. They’re metaphors for repressed anxiety, amplified by late-night scrolling and capitalist burnout. You think your skin’s reacting to wine? No. It’s reacting to the weight of modern existence. You don’t need a cream. You need a retreat. A silent forest. A digital detox. A therapist who doesn’t charge $300/hour. Ivermectin is just a Band-Aid on a hemorrhaging soul.
And let’s not ignore the cultural dimension. In India, rosacea is often seen as a sign of ‘inner heat’-pitta imbalance. Ayurveda recommends cooling herbs like neem and sandalwood. But here? We slap on a $300 tube of cream and call it science. We’ve lost touch with the wisdom of the body. We’ve turned healing into a commodity. The real treatment? Stop consuming. Start listening.
And yet… I get it. I’ve been there. I’ve cried in the mirror. I’ve avoided photos. I’ve canceled plans because my face looked like a traffic light on fire. So yes, use the cream. But don’t stop there. Go for a walk without your phone. Drink water. Breathe. Let your skin breathe too. The mites? They’re just doing their job. You’re the one who needs to change.
And if you’re still using toners with alcohol? Honey. Put it down. Walk away. Your skin isn’t your enemy. The world is. But you? You’re still worthy. Even with the redness.
And if you think this is just acne? You haven’t lived. Rosacea doesn’t care if you’re rich, thin, or ‘healthy.’ It doesn’t care if you work out or meditate. It just… is. And that’s the hardest truth of all.
Jennifer Littler
17 Jan, 2026
As a dermatology nurse, I’ve seen patients quit after 3 weeks because ‘it’s not working.’ The data shows 76% reduction with ivermectin-but it takes 8 weeks to see it. Most people don’t wait. The real failure isn’t the medication-it’s the expectation of instant results in a world that’s trained us to expect TikTok fixes for chronic conditions.
Also, ocular rosacea is massively underdiagnosed. If your eyes burn when you wake up, tell your derm. Don’t wait until you can’t wear contacts. It’s not ‘dry eyes.’ It’s inflammation. And yes, it’s treatable.
Roshan Joy
19 Jan, 2026
From India, here! We have a home remedy: aloe vera gel + cucumber juice, chilled, applied daily. Not a cure, but helps cool the redness. Also, avoid turmeric in face masks-sounds healthy, but it’s a trigger for many. And yes, ivermectin works wonders. I’ve seen patients go from hiding to smiling again. 💚
Matthew Miller
19 Jan, 2026
Wow. So the ‘gold standard’ treatment is a cream that kills mites. Let me guess-those mites are just ‘normal flora’ until you pay $300 for a prescription? This is medical capitalism at its finest. You’re telling me we’ve spent decades treating this like acne, when the real fix is a parasiticidal cream? Why didn’t they just say ‘your skin is infested’ from the start? This is embarrassing.
Alfred Schmidt
20 Jan, 2026
I’ve been on ivermectin for 6 months. I’ve cried. I’ve thrown the tube across the room. I’ve Googled ‘is rosacea contagious?’ at 3 a.m. I’ve cried again. But now? I can go to a party. I can take a selfie. I can look in the mirror without wanting to scream. This isn’t just a cream. It’s my freedom. Thank you to the scientists who made this. And to the doctors who didn’t give up on me.
Michael Patterson
21 Jan, 2026
So… metronidazole is ‘gentler’? More like ‘less effective’ and ‘older.’ Why do doctors still push it? Because they’re lazy? Or because pharma pays them? Ivermectin works better, costs more, so they make you suffer for 3 months first? Classic. Also, ‘azelaic acid’ sounds like a spell from Harry Potter. Why not just call it ‘magic cream’?
Adewumi Gbotemi
21 Jan, 2026
Simple truth: avoid heat, avoid stress, avoid alcohol. Use sunscreen. Be patient. My cousin in Nigeria has it too. He uses shea butter and stays in the shade. He doesn’t have fancy creams. But he’s calm. And his face is calm too. Sometimes, the best medicine is just slowing down.
Alex Smith
22 Jan, 2026
Wait-so you’re telling me that a drug developed for livestock parasites is now the most effective treatment for a human skin condition? And the medical community didn’t even notice until 2014? That’s wild. Also, why does everyone act like this is a new discovery? My grandma in ’98 used sulfur soap. It burned like hell. Worked better than half these creams. We’ve just been overcomplicating it with jargon and price tags.
And don’t get me started on ‘trigger diaries.’ I’ve kept one. Turns out, my face turns red when I’m stressed… which is every day. So… I should stop living? Maybe I should just move to a monastery.