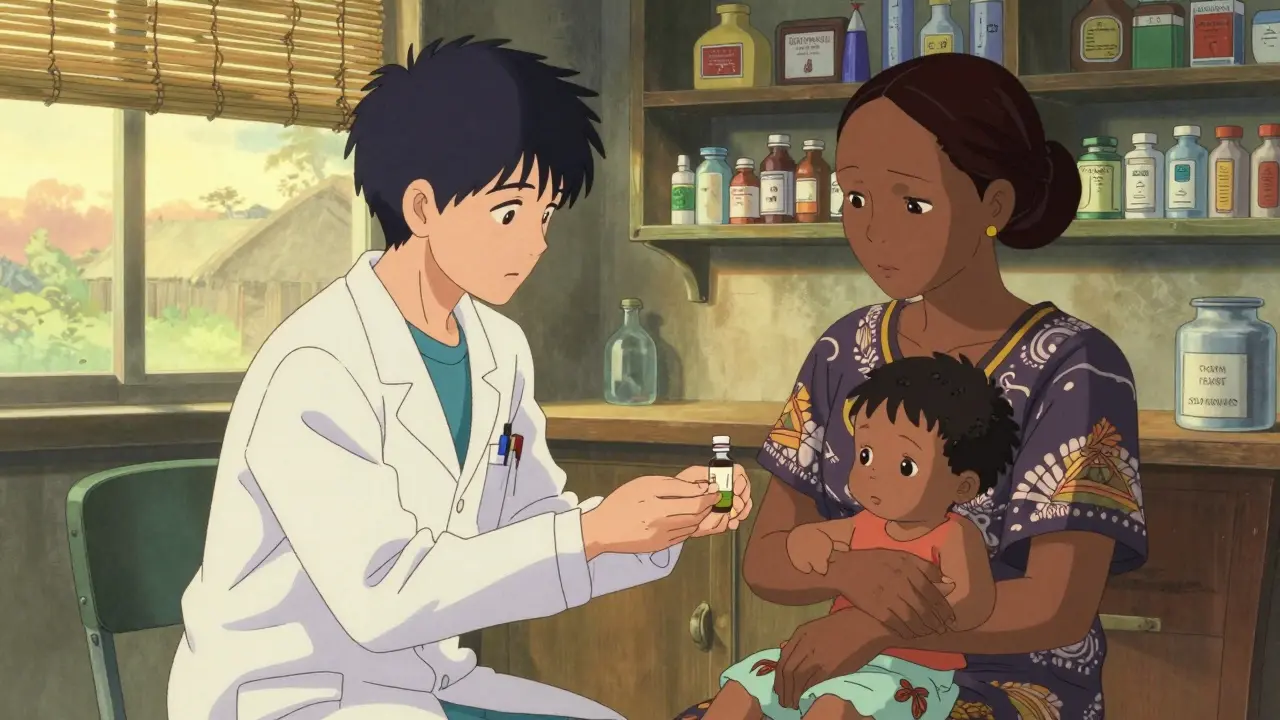
Imagine needing a life-saving drug, but it costs three months’ wages. For millions in low-income countries, this isn’t a hypothetical. It’s daily reality. The answer isn’t more money-it’s generics. These are the same medicines as the branded versions, made without patents, sold for a fraction of the price. Yet, despite cutting drug costs by up to 80%, they still don’t reach most people who need them.
Why Generics Matter More Than You Think
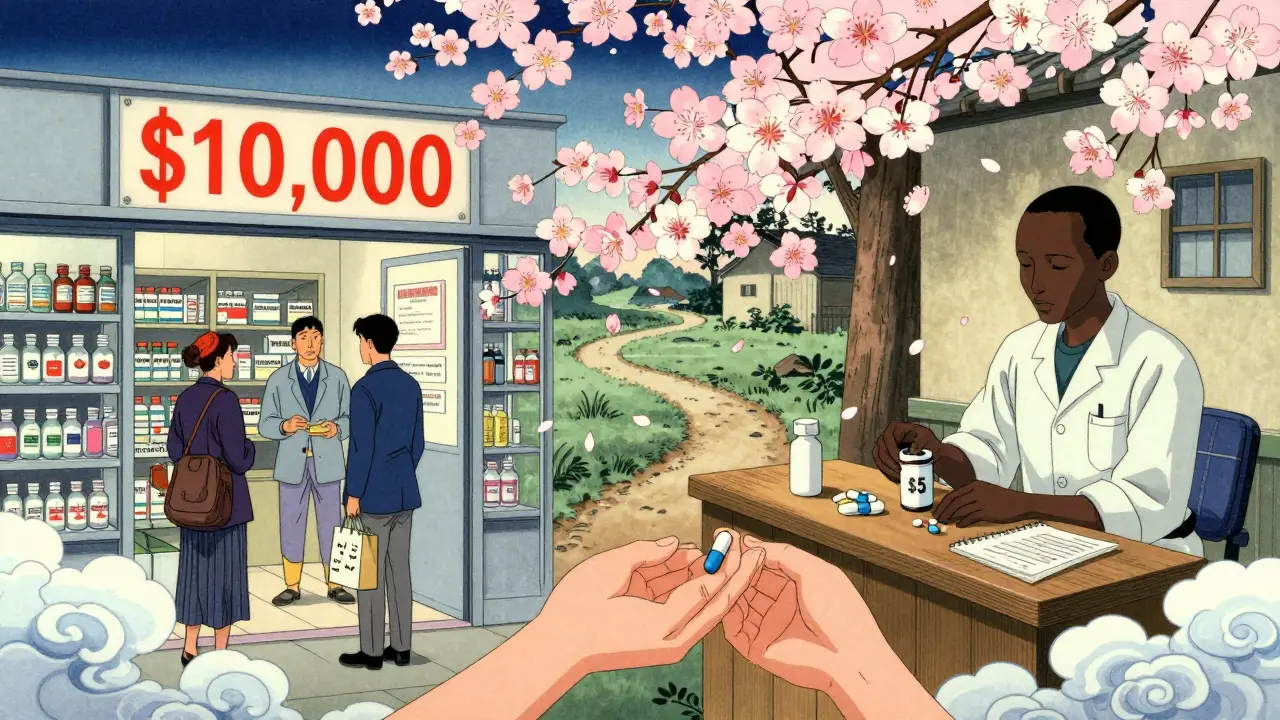
Generics aren’t cheap knockoffs. They contain the exact same active ingredients, work the same way, and meet the same safety standards as brand-name drugs. The difference? No patent. No marketing. No middlemen inflating the price. A course of HIV treatment that once cost $10,000 a year in the U.S. dropped to under $100 in Africa thanks to generic manufacturers like Cipla and Viatris. That’s not a miracle-it’s basic economics. The World Health Organization says 2 billion people lack access to essential medicines. In many low-income countries, people pay out-of-pocket for nearly 90% of their drugs. That means a single prescription can wipe out a family’s savings. Every year, about 100 million people are pushed into extreme poverty just because they got sick. Generics could stop that. But they’re not being used.Why Aren’t Generics Everywhere?
You’d think if generics cut costs so dramatically, they’d be everywhere. But in low-income countries, unbranded generics make up only 5% of the pharmaceutical market by volume. In the U.S., that number is 85%. Why the gap? One reason is trust. Many patients and even doctors in low-income countries worry generics are fake or weak. And while counterfeit drugs are a real problem, the real issue is that many legitimate generics never reach the market. Regulatory systems in places like Nigeria, Bangladesh, or Mozambique are slow, underfunded, and inconsistent. A drug that’s approved in Europe might take two years to clear customs in a rural clinic in Malawi. Then there’s supply chains. A medicine might be made in India, shipped to a port in Kenya, then sit in a warehouse for months because there’s no reliable trucking, no refrigeration, or no one to manage inventory. The WHO says medicine availability in public clinics in many countries is below 80%-the minimum target. In parts of the Western Pacific, it’s dropped even further since 2009.Who’s Making Generics-and Who’s Not Helping
Five big generic companies-Cipla, Hikma, Sun Pharma, Teva, and Viatris-produce 90% of the off-patent drugs needed in low-income countries. They’ve made HIV, TB, and malaria drugs affordable. But here’s the catch: they’re not trying hard enough to reach the poorest. A 2024 analysis by the Access to Medicine Foundation found that these companies had access strategies for only 41 out of 102 essential drugs. And even then, few of those strategies considered whether patients could actually pay. If you’re earning $2 a day, even a $5 generic is too expensive. Yet companies rarely offer tiered pricing, free delivery, or community-based distribution for the most vulnerable. Meanwhile, big pharma companies like Novartis and Pfizer run programs to help low-income countries, but they rarely say how many people actually get the drugs. Transparency is missing. It’s easier to announce a partnership than to track how many children in rural Uganda got their malaria medicine.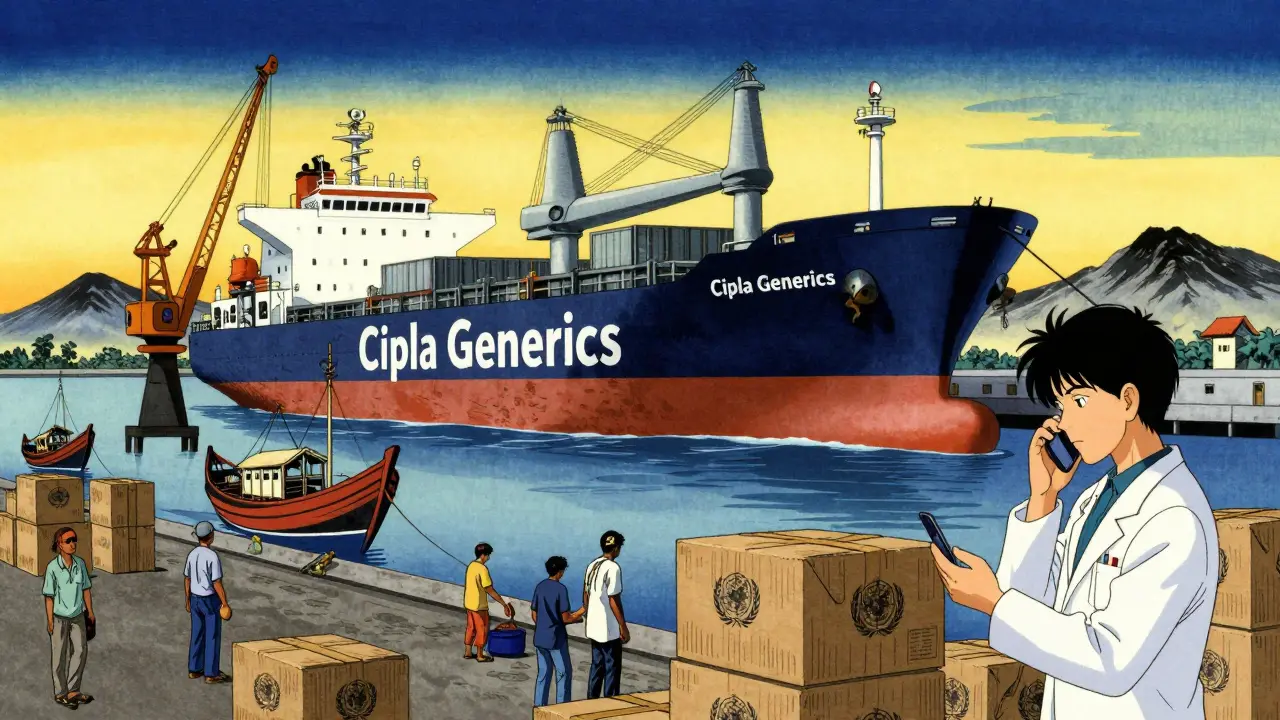
The Real Barriers: Taxes, Tariffs, and Bureaucracy
It’s not just about making the drugs. It’s about getting them through the door. Many low-income countries still charge import tariffs on medicines-sometimes as high as 20%. That’s like adding a tax on救命药. The Geneva Network says abolishing these tariffs alone could slash drug prices by 15-30%. Yet few governments act. Why? Because they need the revenue. But that revenue comes from sick people. Patent laws are another hurdle. Even though the WTO allows developing countries to ignore patents for public health emergencies, many don’t have the legal capacity to do it. They lack lawyers, regulators, or even basic health ministries to push through emergency approvals. And then there’s the lack of investment. In 2001, African Union countries promised to spend 15% of their national budgets on health. By 2022, only 23 of 54 countries had done it. That means clinics run out of medicine. Hospitals can’t afford to hire pharmacists. People die because the system is broke.What’s Working-And How to Scale It
Some places are getting it right. In Rwanda, the government partnered with generic manufacturers and used data to predict drug needs. They now have over 90% availability of essential medicines in public clinics. In Ethiopia, they set up regional drug distribution hubs to cut delivery times from weeks to days. In India, bulk procurement by the government brought down the price of insulin by 80%. The secret? Simplicity. No fancy tech. No billion-dollar apps. Just:- Removing import taxes on medicines
- Fast-tracking generic approvals
- Buying in bulk for public clinics
- Training community health workers to distribute drugs
- Using mobile phones to track stock levels
The Future: Can Generics Save Millions?
The tools exist. The science is solid. The cost savings are proven. What’s missing is political will. If every low-income country eliminated medicine tariffs, streamlined approvals, and invested just 10% more in public health supply chains, millions could get the drugs they need. Even small steps-like training one pharmacist per district or using local warehouses instead of central stockpiles-would make a difference. The real question isn’t whether generics work. It’s whether we care enough to make them work for everyone.Right now, a child in South Sudan can die from pneumonia because the antibiotic costs more than her family earns in a week. That’s not a medical failure. It’s a moral one.
Generics have already saved 100 million lives in the fight against HIV. They can do the same for diabetes, hypertension, asthma, and cancer-if we stop treating access as a charity issue and start treating it as a human right.
What Can Be Done Today?
You don’t need to be a government to help. But if you are:- Remove import taxes on generic medicines
- Set up fast-track approval for WHO-listed generics
- Buy medicines in bulk for public clinics
- Invest in local storage and transport
- Train community health workers to distribute drugs
If you’re a donor, NGO, or global health advocate:
- Push for transparency: demand data on who gets the drugs
- Support local generic manufacturers instead of importing from abroad
- Fund supply chain fixes, not just drug donations
There’s no need to wait for a breakthrough. The cure is already here. It’s just not reaching the people who need it most.





Oladeji Omobolaji
22 Jan, 2026
Man, I seen this firsthand in Lagos-people paying triple for branded antibiotics because the clinic staff didn’t know generics were legit. Some even think the white pills are 'watered down' because they don’t have the fancy logo. It’s not about quality, it’s about trust-and that’s something you gotta build slow, not just print on a label.
Janet King
24 Jan, 2026
The data supporting generic medications is robust and consistently validated by international regulatory bodies. Access barriers are primarily structural and require systemic reform, not merely increased awareness.
dana torgersen
25 Jan, 2026
Wow... I mean... like, think about it-why do we let corporations control life-saving stuff? It’s not medicine, it’s a commodity now, and that’s... messed up. I mean, a child dies because someone’s stock portfolio needs a boost? That’s not capitalism, that’s... that’s... evil? I don’t even know what word fits anymore.
Laura Rice
26 Jan, 2026
I just want to say-this isn’t just about drugs. It’s about dignity. It’s about a mother choosing between feeding her kids and giving her husband his blood pressure pills. It’s about a teenager with asthma who can’t breathe because the inhaler costs more than her school uniform. We talk about ‘health equity’ like it’s a buzzword, but when was the last time you held someone’s hand while they waited for a pill that should’ve been free?
Generics aren’t a Band-Aid. They’re a lifeline. And if we’re still debating whether they’re worth it, we’ve already lost.
Stacy Thomes
26 Jan, 2026
THIS. THIS IS THE MOMENT. We have the power to fix this RIGHT NOW. No magic cure. No billion-dollar vaccine. Just remove the taxes. Just buy in bulk. Just train the local workers. It’s not rocket science. It’s just… human decency. Let’s do it.
Dawson Taylor
28 Jan, 2026
Access to essential medicines is a function of institutional capacity, not merely pharmaceutical availability. The failure lies in governance, not pharmacology.
Andrew Smirnykh
29 Jan, 2026
I’ve worked in clinics across Southeast Asia. The real bottleneck isn’t the drug-it’s the person who has to carry it 30 kilometers on a motorcycle with no fridge. We focus on the pill, but the chain breaks long before it reaches the patient.
Kerry Evans
30 Jan, 2026
Let’s be honest-most of these countries are corrupt. Why should taxpayers in the U.S. fund medicine for governments that steal it? If they can’t manage their own supply chains, why should we care?
Sue Stone
1 Feb, 2026
My cousin in Ghana got her diabetes meds for $2 a month-same pills, same results, just no brand name. She said the only difference was the packaging. People need to stop being scared of plain white pills.
Anna Pryde-Smith
1 Feb, 2026
HOW DARE YOU SUGGEST THIS ISN’T A CRISIS?! People are DYING because some CEO wants a bonus. This isn’t ‘policy’-it’s murder by bureaucracy. And you’re all sitting here talking about ‘supply chains’ like it’s a PowerPoint slide. It’s a funeral.
charley lopez
1 Feb, 2026
The pharmacoeconomic model demonstrates a clear inverse correlation between tariff imposition and therapeutic accessibility. Structural inefficiencies in logistics infrastructure remain the primary impediment to equitable distribution.
Kerry Moore
2 Feb, 2026
Thank you for sharing this. I’ve seen how hard frontline workers fight just to keep a single shelf stocked. The real heroes aren’t the CEOs-they’re the nurses who walk miles to deliver pills because the truck never came.
Sallie Jane Barnes
3 Feb, 2026
My dad was a pharmacist in rural Kentucky. He used to give away meds to people who couldn’t pay. We didn’t have generics back then-but we had heart. We need to bring that back. Not more laws. More humanity.
Susannah Green
5 Feb, 2026
Wait-so if we remove tariffs, fast-track approvals, and buy in bulk, we can cut prices by 50%+? Why isn’t this being done everywhere?! This isn’t complicated. It’s just… ignored. Someone’s making money off this broken system. And we’re letting them.