Every year, millions of people take prescription drugs and over-the-counter medications without issue. But for some, a medication that works for others can cause serious, even life-threatening side effects. The problem? Many of these reactions go unreported. That’s where the FDA’s adverse event reporting system comes in. It’s not just a formality - it’s one of the most important tools we have to keep drugs safe after they hit the market. If you’ve experienced a bad reaction to a medication, you’re not just helping yourself. You’re helping thousands of others who might take the same drug next.
What Counts as an Adverse Event?
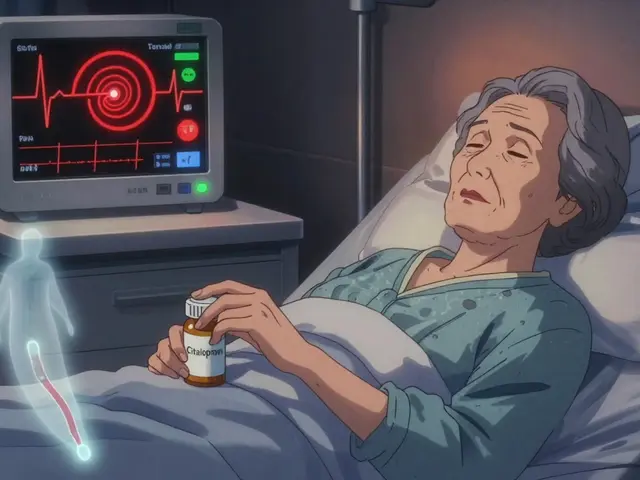
An adverse event is any health problem that happens after you take a medication - whether or not the drug actually caused it. That includes everything from mild rashes and nausea to heart attacks, liver failure, or death. The FDA doesn’t require proof that the drug caused the problem. They just need to know it happened. Even if you think it’s just a coincidence, report it. One report might seem small. But 100 reports of the same issue? That’s a signal.The FDA defines an adverse event as any unexpected experience linked to a drug’s use. This includes:
- Serious side effects (hospitalization, disability, life-threatening)
- Drug interactions you didn’t expect
- Overdoses - even accidental ones
- Withdrawal symptoms after stopping a drug
- Medications that didn’t work when they should have
For example, if you took a common painkiller and developed sudden swelling in your throat, that’s an adverse event. If your blood pressure spiked after starting a new antidepressant, that’s one too. Don’t wait to see if it happens again. Report it now.
Who Can Report?
Anyone can report an adverse event to the FDA - patients, family members, caregivers, pharmacists, nurses, and doctors. But there are two main groups:- Consumers and patients: You can report directly. No special training needed.
- Healthcare professionals: You’re encouraged to report, and in some cases, legally required (like with vaccines under the National Childhood Vaccine Injury Act).
- Drug manufacturers: They must report serious adverse events within 15 days. They use a special electronic system - more on that later.
The FDA gets about 2 million reports each year. Roughly 400,000 come from patients like you. That’s a lot of real-world data you’re helping to collect.
How to Report as a Patient or Consumer
Reporting as a patient is simple. You don’t need to be a doctor. You don’t need to understand medical jargon. Just follow these steps:- Collect basic information. Write down:
- Your name, age, and gender (you can report anonymously if you prefer)
- The name of the drug (brand and generic if you know it)
- The dose and how long you took it
- The date you started the drug and when the problem started
- A clear description of what happened - symptoms, how severe, how long they lasted
- Any other medications or supplements you were taking
- Whether you went to a doctor or hospital
- Go to the MedWatch website. Visit www.fda.gov/medwatch. Click on "MedWatch Online Reporting Form" (Form 3500). This is the official online portal.
- Fill out the form. The form asks for:
- Patient details (age, gender, weight - if known)
- Drug information (name, dose, route - oral, IV, etc.)
- Adverse event description (use plain language: "I felt like my chest was being crushed" instead of "angina")
- Outcome (did you recover? Were you hospitalized? Is it ongoing?)
- Reporter info (your name, phone, email - optional but helpful)
- Upload evidence if you can. You can attach photos of the prescription label, pill bottle, or even the actual medication. This helps the FDA match the report to the right product.
- Submit. Click "Submit." You’ll get a confirmation number. Save it. If the system times out (yes, it happens), you can log back in and resume using that number. Reports are saved for up to three days.
Some people worry about privacy. The FDA doesn’t share your personal info with drug companies. Your report is anonymized before it enters the FAERS database. You’re not being tracked. You’re helping science.
How Healthcare Professionals Report
Doctors, nurses, and pharmacists have a bigger role. You’re not just reporting - you’re adding clinical context that turns a vague complaint into actionable data.Use the same MedWatch online form. But here’s what makes your report more powerful:
- Include lab results (like elevated liver enzymes or abnormal EKGs)
- Attach medical notes or discharge summaries
- Note the timeline - when the drug was started, when symptoms appeared, when they resolved
- State whether the event was expected based on the drug’s label
According to FDA internal data, reports from healthcare professionals are 73% more likely to trigger a safety review than patient-only reports. Why? Because they include objective data. A simple note like "ALT increased from 25 to 420 U/L after 7 days of drug use" tells a story that’s hard to ignore.
What Happens After You Report?
Your report goes into the FDA Adverse Event Reporting System (FAERS), which holds over 30 million reports since 1968. Every month, the FDA analyzes these reports using statistical tools that look for unusual patterns. For example, if 100 people report kidney failure after taking a new diabetes drug, and only 2 reported it with older drugs, that’s a red flag.The system doesn’t prove causation - it finds clues. Then, scientists run follow-up studies. That’s how the FDA discovered the link between fluoroquinolone antibiotics and aortic aneurysms in 2018. That led to a "Black Box" warning - the strongest warning the FDA can issue.
After you submit, you won’t get a call. But your report is still doing work. If enough similar reports come in, the FDA may:
- Update the drug’s label with new warnings
- Require the manufacturer to study the risk further
- Send safety alerts to doctors and pharmacies
- Take the drug off the market (rare, but it happens)
One patient’s report can change how a drug is used nationwide.
What Manufacturers Must Do
Drug companies don’t get to skip this step. If they make a medication, they’re legally required to report serious and unexpected adverse events within 15 calendar days of learning about them. They use a special electronic format called ICH E2B(M), which is standardized worldwide.They must also submit quarterly safety reports for all adverse events. Failure to report can cost companies millions. In 2022, the average fine for a reporting violation was $2.3 million. Over a third of pharmaceutical companies received inspectional warnings related to adverse event reporting that year.
They also have to translate foreign reports into English within 15 days - a huge burden for global companies. That’s why many invest in 24/7 monitoring systems.
Why Reporting Matters - Even If You Think It’s "Not That Bad"
You might think, "My rash wasn’t that bad. It went away." Or, "I’m sure it was just stress." But here’s the truth: the FDA estimates only 1% to 10% of serious adverse events are ever reported. That means for every report they get, there are 9 to 99 more they don’t.That’s why your report matters. A single case of unexplained dizziness might be dismissed. But if 500 people report the same thing after taking the same drug? That’s a signal. And that signal can lead to a warning that saves lives.
Dr. Joseph A. Zoretti, former FDA deputy director, said in a 2022 JAMA article: "FAERS has detected 85% of major drug safety issues within two years of approval." That’s because of reports like yours.

Common Problems and How to Avoid Them
Not all reports are created equal. Here’s what makes a report useless - and how to fix it:- "I took the pill and felt weird." → Too vague. Say: "Within 3 hours of taking 50 mg of sertraline, I had chest tightness, sweating, and blurred vision. Symptoms lasted 6 hours."
- Missing drug name. → Always include brand and generic name. "I took my blood pressure pill" isn’t enough. Was it lisinopril? Amlodipine?
- No timeline. → When did you start the drug? When did symptoms begin? When did they end?
- No lab results. → If you saw a doctor, include blood work or imaging findings. This boosts your report’s value by over 60%.
Reports with full clinical details are 82% more likely to help the FDA identify a real safety issue. Don’t leave out the details.
What’s New in 2026?
The FDA isn’t standing still. In 2023, they launched FAERS Public Dashboard 2.0 - a free, interactive tool that lets anyone explore drug safety data. You can search by drug, symptom, or outcome. It’s not just for experts anymore.By 2024, the FDA will start using AI to scan reports for hidden patterns. They trained the system on 10 million past reports. It’s like having a superhuman researcher reading every single submission.
They’re also working with electronic health records. Imagine if your doctor’s system automatically flagged a rare side effect and sent a report to the FDA - no form needed. That’s the future. And it’s coming fast.
What If You Don’t Report?
If you don’t report, nothing changes. The drug stays on the shelf. Other people keep taking it. Another parent might not know their child’s reaction was linked to a medication. Another senior might keep getting dizzy because no one told the FDA.Reporting isn’t about blame. It’s about awareness. It’s about turning pain into protection.
Can I report an adverse event anonymously?
Yes. The FDA allows anonymous reporting. You don’t need to give your name, phone number, or email. However, providing contact information helps the FDA follow up if they need more details - which can improve the quality of the report and increase its impact.
Do I need to prove the drug caused the reaction?
No. The FDA doesn’t require proof of causation. They only need to know the event happened after taking the drug. Even if you think it’s unrelated, report it. The system is designed to detect patterns across thousands of reports - not to assign blame for one case.
How long does it take for the FDA to act on a report?
There’s no fixed timeline. Individual reports are not reviewed one by one. Instead, the FDA uses software to detect unusual patterns across millions of reports. If a signal emerges - like 500 reports of a rare heart rhythm issue - it triggers a deeper investigation. This can take weeks to months. On average, it takes 217 days from submission to initial safety review, according to the Government Accountability Office.
What if I report and nothing happens?
That doesn’t mean your report didn’t matter. Most safety issues are only identified after dozens or hundreds of similar reports. One report might not change anything today - but it could be the 17th one that finally triggers a warning next year. Your report adds to the evidence.
Can I report side effects from over-the-counter drugs?
Yes. The FDA accepts reports for all medications - prescription, over-the-counter, vitamins, and herbal supplements. Even if a product doesn’t require a prescription, if it caused harm, it should be reported. Many serious reactions come from OTC drugs taken in excess or mixed with other medications.
Next Steps: What You Can Do Today
If you’ve ever had a bad reaction to a medication - even years ago - go to www.fda.gov/medwatch and submit a report. It takes 15 minutes. You might be the reason the next person avoids a dangerous side effect.Share this with friends. Talk about it at the pharmacy. Tell your doctor you care about reporting. Drug safety isn’t just the FDA’s job - it’s ours too.






Rob Turner
15 Feb, 2026
I reported a weird reaction to ibuprofen last year - thought it was just stress, but turns out it was a rare interaction with my blood pressure med. FDA sent me a thank-you email (yes, really). Feels good to know my 15-minute form might stop someone else from ending up in the ER. 🙏
Luke Trouten
15 Feb, 2026
The structural integrity of the FDA's adverse event reporting system is often underappreciated. While anecdotal evidence is inherently noisy, the aggregation of millions of reports creates a robust signal-to-noise ratio that statistical modeling can effectively decode. This is not merely bureaucratic procedure; it is epistemological infrastructure.
Gabriella Adams
17 Feb, 2026
Just wanted to say: if you’ve ever had a bad reaction, REPORT IT. Seriously. I’m a pharmacist and I see so many patients who say, 'Oh, it was no big deal.' But guess what? That 'no big deal' is the first domino. We need every single one. Your report could be the one that changes the label. Don’t be shy. It takes 10 minutes. Do it. 💪
Rachidi Toupé GAGNON
17 Feb, 2026
Reported my cousin’s anaphylaxis to amoxicillin. Didn’t even know you could do it as a family member. Got a confirmation number. Felt like a superhero. 🦸♂️💊 Next time I see a doc, I’m handing them this link. Game changer.
Jim Johnson
18 Feb, 2026
Yo, I used to think this was all just red tape. Then my mom had a stroke after a new statin. We reported it. Two years later, the label got updated. So yeah. Do it. Even if you think it’s nothing. You never know who’s gonna read it next. And trust me - someone’s mom is gonna thank you.
Vamsi Krishna
19 Feb, 2026
Actually, most of these reports are garbage. I’ve worked in pharma compliance. The FDA gets flooded with nonsense - people blaming drugs for migraines, bad hair, or 'feeling sad.' The system is drowning in noise. Real signals get buried. You think your rash matters? Probably not. Unless you’re a doctor with lab results, your report is just static.
Brad Ralph
19 Feb, 2026
So we’re supposed to believe that a 22-year-old’s 'weird headache' after taking NyQuil is somehow as valuable as a cardiologist’s EKG report? 😂 The FDA’s AI is gonna have a nervous breakdown. Also, why is this even on Reddit? This isn’t a 'viral post' - it’s a government form. 🤡
christian jon
21 Feb, 2026
I REPORTED MY SON’S AUTISM DIAGNOSIS AFTER HIS VACCINE - AND THE FDA IGNORED IT! NOW HE CAN’T TALK, AND THEY’RE STILL SELLING IT! THEY’RE COVERING IT UP BECAUSE PHARMA PROFITS > LIVES! YOU THINK THIS IS ABOUT 'ADVERSE EVENTS'? IT’S ABOUT CONTROL! THEY’RE LYING TO YOU! I’VE BEEN RESEARCHING THIS FOR 17 YEARS AND I KNOW THE TRUTH! 🔥🚨💀
Suzette Smith
23 Feb, 2026
Wait, so you’re saying I should report that my headache went away after I stopped taking the pill? That’s not an adverse event - that’s just a placebo effect. You’re overcomplicating this.
Autumn Frankart
23 Feb, 2026
I reported a reaction to metformin last year. Three months later, my phone started ringing nonstop from 'FDA investigators.' They asked if I was a 'plant.' I haven’t slept since. Now I’m being followed. I saw a black SUV outside my house last Tuesday. They’re tracking my glucose levels. This isn’t safety - it’s surveillance. And they’re not even the FDA. It’s the CDC. Or maybe the WHO. Or all of them. I don’t trust any of them anymore. I’m deleting my meds. I’m moving to Alaska.